Total information
Acanthamoeba keratitis is not the only consequence of improper care of contact lenses, but it can confidently be considered one of the most difficult and unpleasant.
The disease occurs in all age groups, but more often in patients from 20 to 40 years old. Ophthalmologists consider such age-related patterns to be the reason for being very busy and regular time pressure (lack of time), due to which certain details of contact lens care can be deliberately or forcedly ignored, which leads to the development of the described disease.
note
Males are affected more often than females. The reason is simple: even being adherents of strict hygiene, men take a more simplistic approach to the issues of proper storage of contact lenses, which risks the amoeba getting into the structures of the eyeball - in particular, into the tissue of its cornea.
The incidence is higher in developed countries due to the fact that patients in ophthalmology clinics more often use the option of vision correction with contact lenses and have more financial opportunities to purchase them. On the other hand, it is assumed that if residents of developing countries (African, Asian) had the financial opportunity to easily purchase contact lenses, then the incidence of acanthamoeba keratitis would be several dozen times higher than in Europe.
Contrary to the stated rules for using contact lenses and preventive explanations from ophthalmologists, the incidence of acanamoeba keratitis associated with improper use of lenses has increased slightly. This is considered a consequence:
- increasing demand for contact lenses;
- using cheap products for their care, which are not always of high quality.
Bibliography
- Centers for Disease Control and Prevention. Brucellosis. Parasites. Link
- Corbel MJ Parasitic diseases // World Health Organization. Link
- Young EJ Best matches for intestinal parasites // Clinical Infectious Diseases. — 1995. Vol. 21. - P. 283-290. Link
- Yushchuk N.D., Vengerov Yu.A. Infectious diseases: textbook. — 2nd edition. - M.: Medicine, 2003. - 544 p.
- Prevalence of parasitic diseases among the population, 2009 / Kokolova L. M., Reshetnikov A. D., Platonov T. A., Verkhovtseva L. A.
- Helminths of domestic carnivores of the Voronezh region, 2011 / Nikulin P. I., Romashov B. V.
An article for patients with a doctor-diagnosed disease. Does not replace a doctor's appointment and cannot be used for self-diagnosis.
The best stories from our readers
Topic: Parasites are to blame for all troubles!
From: Lyudmila S. ()
To: Administration Noparasites.ru
Not long ago my health condition worsened. I began to feel constant fatigue, headaches, laziness and some kind of endless apathy appeared. Problems also appeared with the gastrointestinal tract: bloating, diarrhea, pain and bad breath.
I thought it was because of the hard work and hoped that it would go away on its own. But every day I felt worse. The doctors couldn’t really say anything either. Everything seems to be normal, but I feel like my body is not healthy.
I decided to go to a private clinic. Here I was advised, in addition to general tests, to get tested for parasites. So in one of the tests they found parasites in me. According to doctors, these were worms, which 90% of people have and almost everyone is infected, to a greater or lesser extent.
I was prescribed a course of antiparasitic medications. But it didn’t give me any results. A week later, a friend sent me a link to an article where some parasitologist shared real tips on fighting parasites. This article literally saved my life. I followed all the advice that was there and after a couple of days I felt much better!
Digestion improved, headaches went away and the vital energy that I so lacked appeared. To be sure, I took the tests again and no parasites were found!
Anyone who wants to cleanse their body of parasites, no matter what types of these creatures live in you, read this article, I’m 100% sure it will help you! Go to article>>>
Still have questions? Ask them in our Anonymous group on VK
How to get rid of parasites in a week. The answer is here!
A reliable and effective remedy for combating worms. Removes all parasites in 21 days.
Go to website
Reviews
Read online
Symptoms that 100% indicate parasites! Take the Test.
How to rid your body of life-threatening parasites before it’s too late!
Read more
Website
To get a consultation
The doctor tells how to quickly get rid of parasites for adults and children!
A parasitologist explains what effective methods exist to combat helminths.
More details
Read completely
Comments
Search for cures for parasites
Other tests
We recommend reading
Leishmania braziliensis: description, life cycle, routes of infection and treatment
1 week ago 06/18/202006/18/2020ecoliv94
Isospora belli: description, life cycle, routes of infection and treatment methods
1 week ago 06/18/202006/18/2020ecoliv94
Cryptosporidium parvum: appearance, life cycle, treatment methods
1 week ago 06/18/202006/18/2020ecoliv94
Babesia canis: parasite morphology, life cycle, diseases caused
1 week ago 06/17/202006/17/2020ecoliv94
Causes and development of pathology
The direct cause of the development of the described disease is pathogens from the genus Acanthamoeba - namely:
- culherisom;
- castellanii;
- polyphaga;
- astronyxis.
Also, pathogens of the genus Hartmanelta are detected in patients with diagnosed pathology. But the role of Acanthamoeba in the development of this disease remains decisive, which is reflected in the name of the pathology.
Acanthamoebas are considered free-living microorganisms - during sanitary control they are sown in almost all possible environments. First of all, this is:
- tap water;
- soil of various types;
- reservoirs – in particular, with standing water;
- swimming pools (especially those equipped at home);
- sewerage communications system.
Acanthamoeba was found equally often in tap water in both urban and rural areas. Moreover, they were sown even from an environment that had undergone proper sanitary treatment. In a treated environment, Acanthamoeba manages to survive due to the “dormant” form - the cyst. Thanks to it, the resistance of this infectious agent increases several times (according to some data, several dozen times) under the following conditions:
- too low or high temperatures;
- high blood pressure;
- radioactive and ultraviolet radiation;
- abnormal level of humidity (when staying in the soil);
- the presence of substances with antiseptic properties.
In the form of a cyst, Acanthamoeba maintains a minimum level of vital activity just to survive in unfavorable conditions. In this form, once it enters the human body, it does not come into conflict with his immune system, does not have an irritating effect on it, and therefore does not provoke immune reactions and, accordingly, clinical manifestations.
External receptors of the amoeba, which resides in the form of a cyst, are sensitive to certain environmental parameters. They “catch” changes, and under optimal parameters (in particular, humidity and temperature) they give a signal to “awaken” - the inactive form of Acanthamoeba turns into an active one, which is also called a trophozoite.
note
When Acanthamoeba transforms from a cyst into an active form, its lytic enzymes are among the first to be activated - substances that are capable of breaking down human protein structures in order to penetrate into tissues. High activity of such enzymes in relation to corneal tissues has been noted, which causes the development of acanthamoeba keratitis.
Why do Acanthamoebas become a common cause of damage to the cornea, provoking a specific form of inflammation? The presence of a pathogen and a high level of activity of its enzymes are not enough to cause a disease - the immune system reacts to the pathological agent and destroys it even before it penetrates the tissue. But if contact lenses are not properly cared for (as well as incorrectly selected and used), they lead to injury to the eyeball. Through microtrauma, Acanthamoeba enters the corneal tissue, where it immediately causes a pathological process.
Factors that contribute to the more rapid development of the described pathology are identified. This:
- swimming in a pond or pool;
- using regular tap water to rinse contact lenses;
- storing them in containers that have previously been rinsed with tap water.
Also play a role:
- disorders of the immune system in the form of immunodeficiencies - congenital and acquired;
- the presence of other infectious foci in the body - pathogenic microflora depletes the resources of the human immune system, which are not enough for a timely response to the introduction of Acanthamoeba and the fight against it;
- previous eye diseases;
- regular strain on the organ of vision - work that involves using a computer, poor conditions (lighting, the parameters of which do not meet sanitary and hygienic standards);
- condition after mechanical injury to the eyeball. This applies to both diagnostic manipulations, which, due to careless execution, led to a violation of the integrity of the tissues of the eyeball, and accidental injury;
- previous surgical interventions on the eyeball - especially those that are fraught with prolonged restoration of the cornea;
- regular exposure to conditions of increased smoke and/or gas pollution;
- bad obsessive habits - namely the habit of constantly touching or rubbing your eyes;
- independently carrying out any manipulations on the organ of vision without observing hygiene rules (removal of a foreign body, etc.);
- dry eye syndrome – insufficient amount of tear fluid produced (it is important in order to ensure the proper level of local immunity);
- diabetes mellitus is a disorder of carbohydrate metabolism due to insulin deficiency. Against the background of pathology, small vessels suffer, microcirculation of tissues deteriorates, which provokes a violation of their regenerative abilities;
- disruptions of thyroid hormones - hypothyroidism (decreased their synthesis) and hyperthyroidism (increased their amount in the blood). The mentioned hormones are responsible for metabolic (metabolic) processes in tissues - against this background, local immunity and the regenerative ability of corneal tissues suffer;
- use of low-quality or expired cosmetics (eye shadows, mascara, creams for application to the periorbital area);
- smoking. Nicotine provokes a constriction of blood vessels, due to which blood flow through them deteriorates, as a result of which the blood supply to tissues suffers. They receive less oxygen and nutrients than necessary, so they recover less well - including the cells of the immune system that respond to infectious resistance (resistance) at the local level.
In order for Acanthamoeba to provoke the development of a pathological process, it is necessary that a certain amount of the pathogen enters the body (in particular, the tissue of the cornea). This factor explains the fact that some people experienced acanthamoeba keratitis upon contact with contaminated water, while others avoided it.
Having penetrated the tissue of the cornea, the infectious agent triggers a series of pathological changes - first of all, an inflammatory reaction. There are four stages of the described disease:
- the first is superficial epithelial keratitis;
- the second is superficial epithelial punctate keratitis;
- third – stromal ring keratitis;
- the fourth is ulcerative acanthamoeba keratitis.
In the first stage of the described pathology, corneal edema appears. It has a “local” character - it manifests itself in the form of a limited focus of a circular shape. Most often, such swelling occurs in the central part of the cornea.
In the second stage, clouding appears and progresses at the site of swelling; the cornea in this place is infiltrated (literally “soaked”) with immune cells. Also, small compactions in the form of white or gray dots appear over the entire surface of the cornea. In addition, the nerve structures of the cornea thicken and become inflamed (a peculiar form of neuritis, an inflammatory lesion, occurs) - making them easy to recognize during an ophthalmological examination.
In the third stage, a peak of acanthamoeba activation is observed - it vigorously absorbs epithelial cells of the cornea. At the same time, acanthamoeba releases toxins and waste products that irritate the corneal tissue, causing an inflammatory process to develop in them. In addition, the connective tissue fibers that form the basis of the cornea (stroma) undergo the following changes:
- are impregnated with immune cells “sent” by the immune system to eliminate the pathological process;
- swelling.
Also, as the disorders progress, iritis occurs - an inflammatory lesion of the tissues of the iris, which develops due to the spread of the pathological process to it.
In the fourth stage of acanthamoeba keratitis, the integrity of the cornea is compromised. Corneal defects begin as superficial erosions that progress to deep ulcers. At this stage, complications of the described disease begin to develop.
note
Acanthamoeba keratitis can be either unilateral or bilateral. Often, one eye is affected first, and the second is drawn into the pathological process only after a few weeks or even months. The disease begins acutely, but then becomes chronic. In some cases, the development of a primary chronic process with a protracted course is observed.
Causes of acanthamoebiasis
Acanthamoeba is a single-celled organism that lives in contaminated water and wet soil. Can be found in well and tap water, and Jacuzzis.
When it gets on the damaged surface of the cornea, acanthamoeba causes the development of infection - keratitis.
The causative agent of acanthamoeba keratitis is the simplest single-celled organism - acanthamoeba, which lives in the aquatic environment. Acanthamoeba can be found not only in water from artificial or natural reservoirs, but even in tap water that has undergone the necessary cycle of purification and disinfection.
When taking a shower or bath, swimming in open water or swimming pools, contact lenses must be removed.
- photokeratitis (in welders)
— disruption of innervation when 1 branch of the trigeminal nerve is damaged.
Most cases of Acanthamoeba keratitis occur in people who wear lenses to correct their vision. However, the reason for this is not modern means designed for storing lenses, but neglect of the rules of hygiene and use of contact lenses.
Despite the increased incidence of acanthamoeba keratitis, this disease is still considered quite rare, but extremely dangerous, as it can lead to complete destruction of the lens.
Acanthamoebas, which are classified as simple amoebas, often live in bodies of water. These microorganisms, in addition to their natural habitat, can lead a parasitic lifestyle.
Their main habitat is the eyes of fish and animals. The eyes are an ideal habitat for this species of amoebas, as they contain an ideal nutrient medium.
In addition, the extreme saturation of people's eyeballs with blood vessels contributes to eye damage.
Among the free-living pathogenic amoebae of the genus Acanthamoeba, 6 species are dangerous to humans: A. hatchetti (cause eye damage), A. palestinensis and A. astronyxis (cause damage to the central nervous system), A. polyphaga, A. Culbertsoni, A. castellanii (cause various damage , including skin). During the life cycle of amoebas of the genus Acanthamoeba, they pass through a vegetative stage (trophozoite) and a cyst stage.
Acanthamoeba are aerobic organisms that live in soil, standing freshwater in natural and artificial reservoirs, especially contaminated by wastewater discharges. In addition, single-celled protozoa live safely in tap water, sewage systems, and water from heating pipes.
The increase in the Acanthamoeba population is facilitated by water temperatures above 28°C and the presence of various organic substances in it. If the ambient temperature decreases or the reservoir dries out, the Acanthamoebas encyst.
In the cyst state, parasites tolerate fluctuations in temperature and pH, and exposure to antiseptics and disinfectants.
Symptoms of acanthamoeba keratitis
The clinical picture depends on the stage of the disease.
When pathology occurs, the following symptoms appear:
- discomfort;
- feeling of a foreign body in the eye;
- progressive deterioration of vision.
Discomfort in this case appears when the eyes are closed under the upper eyelid and manifests itself in the form of vague unpleasant sensations.
If no therapeutic action has been taken, the following disorders develop:
- pain;
- hyperemia;
- blepharospasm - closing of the eyelids;
- lacrimation;
- Photophobia is a painful reaction to irritation by light.
The characteristics of pain are as follows:
- by localization - throughout the eyeball;
- in terms of distribution - irradiation as such is not typical;
- by nature - aching-pressing, with the formation of erosions and ulcers - cutting;
- in terms of severity - at first insignificant, then they increase, becoming pronounced;
- according to occurrence - first periodic, then constant, including disturbances at night.
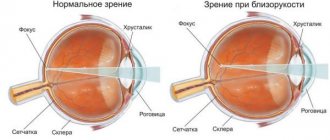
As a final result, the pain progresses to a level of very intense, often unbearable, and vision deteriorates until it is completely absent (even the inability to distinguish light). The main cause of visual impairment is a pathological change in the structure of the cornea, which is one of the optical media of the organ of vision.
Classification features
Acanthamoeba keratitis is divided into four main stages:
- Stage 1 is characterized by superficial epithelial keratitis. In this case, epithelial edema occurs in the central part of the cornea. Less common in paracentral zones.
- Stage No. 2 has a superficial epithelial punctate form. Infiltration of the cornea is more pronounced, and rapid clouding is noted. Upon examination, gray or white nodules are observed that protrude on the epithelium. In addition, nerve trunks can be seen in the stroma, and the patient experiences significant pain.
- Stage No. 3 is the ring stromal form of keratitis. In this case, amoebas begin to intensively feed on the epithelial cover of the cornea, resulting in inflammatory processes in the upper layers of the stroma. The cornea undergoes further clouding, and severe swelling of the stroma is noted. This provokes the development of iritis.
- Stage No. 4 refers to ulcerative keratitis, as the cornea becomes covered with ulcers. As consequences and complications, iritis, hypopyon, iridocyclitis, scleritis, glaucoma and other diseases occur.
Diagnosis of acanthamoeba keratitis
Identifying inflammatory changes in the tissues of the cornea is not problematic, but making an accurate diagnosis taking into account the causative factor is only possible thanks to additional research methods. In general, patient complaints, medical history data, and the results of physical, instrumental and laboratory research methods are equally informative for diagnosing acanthamoeba keratitis.
It is important to clarify such details of the anamnesis as:
- the fact of patient contact with water from various open sources - reservoirs, swimming pools;
- long-term use of contact lenses;
- confirmation of improper care;
- use of low-quality contact lens care products.
A physical examination makes it possible to find out the following nuances:
- upon examination - persistent redness of the eyes, the patient’s painful reaction to light, increased production of tears, regular attempts to rub the eyes;
- upon palpation (palpation) - noticeable pain when pressing through the drooping upper eyelid onto the eyeball.
What instrumental research methods are used to detect acanthamoeba keratitis? This:
- computer keratometry - during it, the refractive power and curvature of the cornea are measured;
- pachymetry – optical (using a slit lamp) or ultrasound (using an ultrasound machine) determination of the thickness of the cornea. Its results reflect the degree of corneal dystrophy;
- Corneal microscopy is a microscopic study of its tissues. Its varieties are endothelial and cofocal mycoscopy. In the first case, photographs are taken of the surface layer of the cornea, in the second, the structure of its different layers is studied. When carrying out this research method, the depth of destruction of the cornea and the swelling of its components are assessed;
- optical coherence tomography of the cornea (OCT) – during this procedure, images of all individual layers of the cornea are obtained, from which their characteristics can be studied;
- Diaphanoscopy is the study of the cornea by shining through the eye with transmitted light. It is carried out with an electric ophthalmoscope with a special attachment that generates light;
- visometry – determination of visual acuity. It is carried out using special tables with symbols decreasing in size, which the patient must name (letters or figures);
- corneal algesimetry is a special test to assess its sensitivity. It is informative if degenerative-dystrophic processes in the cornea are suspected. The simplest method is to touch the cornea with a piece of cotton wool; a more complex and accurate method is to use an optical-electronic esthesiomer (literally “sensitivity meter”).
The following laboratory research methods are informative in the diagnosis of acanthamoeba keratitis:
- general blood test - the inflammatory process is indicated by such a nonspecific indicator as an increase in the number of leukocytes (leukocytosis) and ESR;
- bacterioscopic examination - a scraping from the cornea is examined under a microscope, destroyed cells are identified in it, the pathogen is identified;
- bacteriological examination - a scraping from the cornea is inoculated onto special nutrient media; the pathogen is determined based on the characteristics of the grown colonies.
Complications
Acatnamebic keratitis is most often complicated by diseases and pathological conditions such as:
hypopyon - purulent discharge accumulated in the lower part of the anterior chamber of the eye (the space between the cornea and the iris);
- scleritis is an inflammatory lesion of the deep layers of the sclera (the outer dense connective tissue membrane of the eyeball);
- increased intraocular pressure;
- cataract – clouding of the lens;
- perforation of the cornea;
- visual impairment.
Treatment of acanthamoeba keratitis
Acanthamoeba keratitis is treated with conservative and surgical methods.
Conservative therapy is applicable in the initial stages of the disease and with further progression, but without signs of complications. This involves treatment:
- general;
- local.
The basis of general treatment is the following:
- antifungal drugs - their effectiveness in the treatment of the described disease has been proven. Used in advanced cases;
- painkillers – prescribed for severe pain;
- antibacterial agents - indicated for the prevention and treatment of secondary infections.
The main one is local treatment (usually in the form of eye drops). Patients are prescribed:
- washing the eyes with antiseptic solutions;
- antifungal drugs;
- antibacterial agents;
- glucocorticosteroids—they are usually used in the treatment of prolonged forms of acanthamoeba keratitis.
Surgical treatment is used in case of complications, namely:
- corneal ulcer;
- its perforation.
In this case, plastic surgery of the damaged cornea is performed in different ways.
Prescriptions in the postoperative period are as follows:
- limitation of visual and physical activity;
- a nutritious diet - for the fastest healing of postoperative corneal damage;
- use of alternative methods of vision correction.
Symptoms and signs
Severe pain that does not correspond to the nature of the corneal lesion is a characteristic early symptom.
Clinical characteristics of acanthamoeba keratitis
| Medical history data (risk group) | Typical clinical signs |
|
|
The infectious inflammation in question occurs in a sluggish mode. Treatment with therapeutic agents is difficult. Relatively rarely, the disease is acute.
The following symptoms are distinguished:
- severe corneal swelling;
- severe pain that does not correspond to its visible changes;
- photosensitivity;
- sensation of a foreign body;
- blurred vision.
Prevention
The main measures to prevent acatamoebic keratitis are:
- correct use of contact lenses and careful care of them according to recommendations;
- refusal to swim in bodies of water with standing water;
- visiting only proven swimming pools;
- preventive examinations by an ophthalmologist.
The basis for the correct use of contact lenses and proper care for them are the following recommendations:
- use only certified storage solutions;
- compliance with the terms of use of lenses;
- use of lenses from reputable manufacturers known on the market;
- compliance with hygiene rules when putting on contact lenses.
Prevention
The prognosis for acanthamoeba keratitis is complex - this disease is difficult to treat, and it is usually long-term. Treatment difficulties are aggravated when irreversible changes occur in the cornea.
The prognosis worsens when complications occur.
Kovtonyuk Oksana Vladimirovna, medical observer, surgeon, consultant doctor
2, total, today
( 74 votes, average: 4.08 out of 5)
Aniridia – absence of the iris
Eye pain: possible causes and treatment
Related Posts
Forms
The infectious-inflammatory process of corneal tissue caused by Acanthamoeba keratitis is chronic and does not respond effectively to conservative therapy. The course of the disease in a rapid form, in which active destructive processes of the cornea occur, is rarely recorded.
The stages of the disease are divided depending on the depth of damage to the cornea by Acanthamoeba. Acanthamoeba keratitis can manifest itself in stages, there are several stages:
- superficial epithelial keratitis;
- superficial point;
- stromal ring-shaped;
- ulcerative;
- keratoscleritis.