0
Author of the article: Marina Dmitrievna
2017.10.24
71
Vessels
The disease of central vein thrombosis is classified according to the ICD-10 class code H30-H36. In practice, the disease represents a pathological change in the central retinal vein. As a separate disease, it rarely develops; most often it is an additional concomitant disease to pathological changes against the background of impaired circulation and functional blood clotting. Atherosclerosis, hypertension, systemic vasculitis, diabetes mellitus, thrombophilia of various etiologies are pathologies that contribute to the progression of the disease “thrombosis of the central retinal artery.”
Pre-existing diseases provoke thickening of the vascular walls of the retina, which leads to pressure from other adjacent veins. The process prevents full blood flow, and clots form at the site of compaction. The stagnation phenomenon creates a reverse flow of blood by penetrating into the capillaries, which significantly increases IOP. The continued onslaught of blood leads to rupture of the vascular wall and hemorrhage into the retina with the formation of a swollen area. The disease with thrombosis has dangerous complicating factors and often leads to visual disability - complete blindness.
The main risk group is the elderly. The etiology of the disease in the younger generation occurs in 30% of recorded cases as a complication of progressive focal viral infections.
Retinal thrombosis - how it happens
The disease is not an independent pathology, but develops as a concomitant deviation of the underlying disease.
Definition of disease
Retinal vein thrombosis is a circulatory disorder in the vascular system of the eyes and their branches. Most often they occur in older people and have causes unrelated to the visual organs.
The disease has several stages of development:
- Prethrombosis. The onset of the problem is accompanied by dilation of the veins, changes in their shape and quality of patency. Often the patient at this stage experiences periodic “fogging.”
- Initial thrombosis. Visible symptoms become more noticeable, and small hemorrhages appear on an ongoing basis. The patient may experience deterioration in the quality of vision, the appearance of fog and optical effects.
- Retinopathy. At this stage, abnormal proliferation of blood vessels, swelling, deterioration and loss of vision due to blockage of blood vessels and veins are often observed.
In addition, there are two types of thrombosis:
- Ischemic. With this form, blood circulation is seriously impaired, constant swelling and hemorrhages are observed.
- Non-ischemic. The retina is practically not affected, the quality of vision often does not change.
After treatment, the disease can relapse, repeating each stage again.
Stages of disease development
- Prethrombosis. Due to blood stagnation, the affected vein expands, and tortuous, dark vessels form on the surface. Often the appearance of edema and thread-like small hemorrhages. The first stage of thrombosis is asymptomatic, and patients may perceive temporary blurred vision as a malaise due to overexertion.
- The second stage is characterized by obvious damage to the venous walls; streak-like threads of hemorrhages spread to the entire retina. An increase in vascular permeability forms transudative edema. Impaired visual perception becomes noticeable, patients complain of the appearance of “spots” and “dark spots”.
- Third stage. Progressive thrombosis is accompanied by atrophic or degenerative changes in the affected retina.
Retinal venous occlusion is the cause of blood clot formation in the eye. The development of the disease cannot be ruled out due to thickening of the arterial walls compressing the walls of the veins.
Damage to the vascular walls occurs through the release of blood flow from the vascular bed and is associated with oxygen starvation of the blood circulation. The phenomenon creates recurrent retinal lesions, which is a direct consequence of the complicating factor. Ischemic microtrauma causes an increase in endothelial production to form a new vascular branch. The postthrombotic danger of thrombosis is hemorrhage in the retina with the development of neovascular glaucoma.
Causes
Very often, the causes of thrombosis are diseases not related to the organs of vision. Among the most common reasons:
- Arterial hypertension;
- Atherosclerosis;
- Diabetes;
- Infectious diseases of various types;
- Increased pressure inside the eyes;
- Swelling of the optic nerve;
- Tumors.
The risk group, as a rule, consists of people leading a sedentary lifestyle, suffering from excess weight, heart disease and pathologies of the endocrine system.
Causes
The main factors that can provoke deep vein thrombophlebitis are:
- Infectious pathogens
- Injuries and damage to tissues and bones,
- Impaired tissue nutrition and development of aseptic inflammation,
- Introduction of a chemical irritant into the vessels of the lower extremities,
- Long-term use of hormonal drugs or pregnancy,
- Increased blood clotting.
With diseases such as vasculitis, periarthritis or Bruger's disease, the risk of thrombosis of the veins of the lower extremities increases by approximately 40%. Vascular disease can be triggered by addiction to smoking and alcoholic beverages, problems with the cardiovascular system, as well as excess weight, which leads to obesity.
Possible complications
People suffering from thrombosis of the central retinal veins, without timely diagnosis and treatment, risk losing their vision without the possibility of its restoration. With improper and insufficient treatment, as well as in the absence of control after medical intervention, the pathology can recur. Constant monitoring by your doctor is especially important for people at risk. In addition, new problems may arise: glaucoma, systematic bleeding, nerve atrophy, retinal dystrophy.
Features of central retinal vein thrombosis. Treatment measures
Sometimes the blood vessels in the eyes become clogged with blood clots. At this point, the blood returns to the capillaries. The pressure in them increases. Retinal hemorrhage and swelling occur.
This characteristic refers to central retinal vein thrombosis, which is otherwise called venous stasis retinopathy.
The disease leads to irreversible changes of a degenerative and atrophic nature, which is why treatment rarely has positive results.
ICD-10 code
H34 Occlusion of retinal vessels.
Reasons for the development of thrombosis
Most often, thrombosis of the central retinal vein manifests itself as a consequence of general diseases of the body that affect blood clotting. It is rarely detected as an independent disease.
The initial cause of thrombosis is the disruption of blood flow and the appearance of blood clots in the vessels, caused by compression of the vein adjacent to the compacted artery with thickened walls.
There are other reasons leading to the onset of the pathological process. Among them:
- Infection of the body.
- Ophthalmic hypertension.
- Formation of papilledema.
- Intraocular neoplasms.
- Swelling and formation of infiltrates on the soft tissues of the orbit.
- Having excess weight.
- Disturbances in the endocrine system.
- A lifestyle with limited movement.
- Addiction to alcoholic drinks.
Thrombosis of the central retinal vein in most cases is found in people whose age has exceeded the 65-year mark. According to statistics, in every 10th case, both eyes are affected.
If we talk about the susceptibility of young people to the disease, then in them it is detected as a complication after infectious diseases or inflammatory processes in the nasopharynx.
In rare cases, factors leading to thrombosis are blood cancer or a disorder in the functioning of the hematopoietic organs.
Stages of pathology formation
At the time of development, thrombosis goes through several stages:
1st. Prethrombosis. Visually the disease does not manifest itself in any way. It can only be detected during an ophthalmological examination. During examinations, the doctor may notice that the blood in the veins is stagnating. This is indicated by the condition of the blood vessels. The veins become wider and change in structure. Swelling occurs in the area of the macula, and sometimes hemorrhage appears.
2nd. Initial thrombosis. It manifests itself in the form of cloudiness, spots and flickering before the eyes. Examining the eyeball, the doctor detects hemorrhages in the retina and swelling of the optic nerve head. Gradually, vision indicators fall.
3rd. Retinopathy itself. Characterized by resorption of minor hemorrhages. During this period, the retina undergoes degenerative and atrophic changes. Over the course of 2 months, blood vessels grow throughout the retina. Many parts of the visual system lose their functionality, causing vision to deteriorate.
https://www.youtube.com/watch?v=Q9JEJH5yvdQ
Each stage of the disease has its own characteristic symptoms. However, there are a number of general signs characteristic of thrombosis at any stage of the disease.
Symptoms of the disease
The symptoms of thrombosis are associated with the size of the area covered by the pathology and the presence of additional vascular branches. Most often, the following signs indicate the formation of blood clots:
- the image appears blurry;
- the degree of visual acuity decreases;
- objects are projected in a distorted form;
- Various visual defects are observed.
Thrombosis is usually localized in the area of one eye. Most often, its symptoms make themselves felt during sleep at night. Waking up, a person discovers vision problems that are not accompanied by pain.
Thrombosis of the central vein leads to changes in the fundus. During diagnosis, hemorrhages located as streaks and swelling are detected.
The clinical picture and treatment regimen for central retinal vein thrombosis may look like this:
Can there be complications?
Often, after treatment, central vein thrombosis reappears. It is called recurrent. The disease is difficult to treat and it is impossible to completely restore vision with this pathology. In any case, thrombosis leads to the formation of defects in the fundus. They are expressed as follows:
- Glaucoma.
- Degenerative changes in the retina.
- Atrophic changes in the optic nerve.
- Decreased vascular functionality, provoking the development of uveitis and iridocyclitis.
- Partial limitation of the ability to see or permanent blindness.
The development of complications is influenced by the general condition of the body, the presence of concomitant diseases of the visual organs, the efficiency and quality of treatment.
Thrombosis can affect a person's general condition. He may experience pain in the head and heart, notice an increase in blood pressure and dizziness. One of the cases of complications of the disease was described by an Internet user as follows:
Diagnosis of central retinal vein thrombosis
The main study aimed at identifying central retinal vein thrombosis is ophthalmoscopy. Having examined the condition of the fundus, the doctor can already make the correct diagnosis. However, to compile the most complete clinical picture, he resorts to the following studies:
- Determining the degree of visual acuity.
- Measuring intraocular pressure.
- Determination of the boundaries of the field of view.
- Determination of the retinal photosensitivity threshold.
- Biomicroscopic study of the condition of the eyeball.
- Study of the structure of the retina.
- Identification of the condition of blood vessels.
The next stage of diagnosis is to identify common diseases of the body that provoke the formation of blood clots in the retinal vein. Based on the results obtained, therapeutic measures are carried out. You can learn about diagnostic methods and prognosis of thrombosis from the comments:
How to cope with the disease
Treatment measures are carried out immediately after thrombosis is detected. If their implementation is delayed, this can lead to aggravation of the pathological condition and the occurrence of complications. First of all, conservative therapy is carried out using the following medications:
- Reduced blood pressure. Drugs that have this effect are injected into a vein (Dibazol) or into a muscle (Lasix), dropped into the eyes (Timolol), or placed under the tongue (Phenigidine or Nifedipine).
- Restoring blood flow. Within 7-14 days, injections of Plasminogen or direct anticoagulants are injected into the eye.
- Preventing the recurrence of the disease. Aspirin or Plavix are prescribed. During the period of their administration, the level of blood clotting is monitored.
- Reducing swelling and fighting inflammatory processes. Injections are made under the eyes or hormonal drugs are administered intravenously.
- Improved blood circulation. Reopoliglyukin and Trental are used.
- Replenishment of vitamin deficiencies. Ascorbic acid and vitamin B are taken.
Antispasmodics and angioprotectors are also prescribed. After completing conservative therapy, it is necessary to perform laser coagulation of the retina.
Possible complications during treatment
During treatment of central retinal vein thrombosis, the following side effects are possible:
- Poor tolerance of medicinal components.
- Formation of bleeding.
- Recurrence of macular edema.
- Retinal detachment and hemorrhages leading to blindness.
Such phenomena appear if the patient does not follow the doctor’s recommendations and refuses to be observed by him. If you start treatment in a timely manner and do not resort to independent attempts to get rid of the disease, the prognosis will be favorable.
Preventive measures
You can prevent the development of central retinal vein thrombosis if you take into account the following tips:
- Stop smoking and drinking alcohol.
- Adjust your daily diet so that your body receives enough nutrients.
- Don't forget about daily physical activity.
- Perform eye exercises aimed at developing the ciliary muscle.
- Monitor your blood pressure.
Another step towards reducing the risk of retinal vein thrombosis is timely treatment of cardiovascular diseases and periodic visits to an ophthalmologist.
Source: https://VseProGlaza.ru/bolezni/tromboz-centralnoj-veny-setchatki/
Treatment
At home, it is almost impossible to get rid of the problem at any stage. Therefore, observation by an ophthalmologist is necessary.
Diagnosis is made using the following methods:
- Initial comprehensive examination;
- Ophthalmoscopy;
- Biomicroscopy;
- Visometry;
- Perimetry;
- Tomography.
Checking your blood pressure and reviewing your medical history to determine the cause are also necessary. After a comprehensive examination, treatment is prescribed.
By medication
The most important drugs for the treatment of central retinal vein thrombosis are supportive and blood clot-dissolving drugs. Most often prescribed:
- Fibrinolytics. Restores the integrity of blood vessels.
- Hormonal drugs.
- Medicines that lower blood pressure.
- Angioprotectors.
- Vitamin complexes.
- Antiplatelet agents. Reduce the risk of relapse.
- Antispasmodics.
Drugs that relieve swelling and inflammation, and vascular strengtheners may also be prescribed.
The use of traditional recipes to treat the disease can be dangerous to vision and life. It is best to include an additional therapeutic factor in improving the quality of life and nutrition, as well as feasible physical activity.
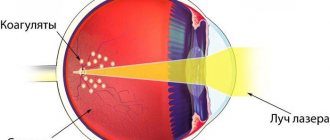
Surgically
One of the most effective methods of treating thrombosis is laser coagulation. Using a laser, blood vessels are coagulated and blood clots are dissolved. As a rule, the technique is applied after drug treatment.
Laser coagulation procedure
Treatment of the disease
Thrombosis of the blood vessels of the eye is eliminated with the help of drug therapy. In some cases, surgery is required. The measures taken are aimed at preserving the vision of the eye.
Treatment involves taking the following medications:
- Phenigidine or Nifediline are prescribed to lower blood pressure. Intramuscular injections with Lasix are also given. Timolol drops are instilled directly into the eyes.
- To eliminate pain, Papaverine and No-shpu are prescribed.
- In order to normalize blood flow, fibrinolytics are prescribed.
- To eliminate the inflammatory process and remove swelling, you need to do droppers with Dexon.
- To prevent relapses, antiplatelet agents are prescribed - Plavix and Acetylsalicylic acid.
The patient remains in the hospital for 2 weeks. After treatment, he must follow the recommendations of specialists. The lack of positive dynamics during drug therapy is a reason for surgical intervention.
The problem is eliminated by performing laser coagulation of the retina. A re-diagnosis is carried out several months after the operation.
According to the international classification, thrombosis of the central nervous system of the eye has the ICD code 10-H 34.8.
Prevention
The basis for preventing blood clots is treating the diseases that can cause them. It is also recommended to lead an active and healthy lifestyle, as well as monitor your blood pressure. In addition, it is important to conduct a routine examination with doctors in various fields, including an ophthalmologist.
Exercises for strabismus
Keratoconjunctivitis: symptoms and treatment of the disease are presented here.
What is anisocoria https://eyesdocs.ru/zabolevaniya/anizokoriya/prichiny-raznyx-zrachkov-u-vzroslyx.html
Diagnosis and treatment of the disease
For thrombophlebitis, doctors prescribe treatment based on the diagnostic results obtained. Treatment includes:
- drug therapy;
- surgical intervention.
Patients with deep phlebothrombosis of the leg (i.e., distal to the popliteal vein system) are managed conservatively in an outpatient setting. All other patients are treated in a surgical hospital • Strict bed rest is prescribed for 7–10 days with the affected limb elevated. Thermal procedures are contraindicated.
Patient management • Bed rest for 1–5 days, then gradual restoration of normal physical activity with refusal of long-term immobilization • The first episode of deep phlebothrombosis must be treated for 3–6 months, subsequent episodes - at least a year • During the administration of heparin i.v. c determine the blood clotting time.
If 3 hours after administration of 5000 units the coagulation time exceeds the initial one by 3–4 times, and after 4 hours by 2–3 times, the administered dose is considered sufficient. If blood clotting has not changed significantly, increase the initial dose by 2500 units.
conclusions
The appearance and development of thrombosis of the central veins and vessels of the retina can cause a lot of trouble and reduce the ability to see well. The likelihood of a recurrence of the problem further complicates the task and makes constant medical monitoring of your health necessary. However, with a healthy lifestyle and proper treatment, the disease does not recur. And its prevention will help keep your visual organs healthy for the rest of your life.
Also read about what papilledema and temporal arteritis are.
How to get rid of thrombosis of the central veins of the retina and what is the ICD 10 code for the disease
The vascular network permeates the entire human body and brings blood to every cell. Vascular pathologies can occur in any organ and lead to characteristic consequences and disruptions in its functioning.
The organs of vision are no exception. A condition called thrombosis most often occurs in the veins of the lower extremities, but in some cases it affects the central retinal vein. What needs to be done to preserve vision and how to suspect pathology in time?
Epidemiology
Thrombosis of the central veins of the retina occurs in approximately 2 people out of 1000. The disease mainly affects people over 40 years of age, which is explained by age-related changes and other causes of this pathology.
Central retinal vein thrombosis is more common in people with glaucoma. With age, the incidence rate increases even more.
According to studies, it was found that most people with this disorder developed extraocular vascular problems.
In approximately 18% of patients with blocked veins in the eye, after some time the other eye was also affected. In this case, the problem can occur in both veins and arteries.
Scheme of step-by-step patient management
Many diseases in ophthalmology are accompanied by similar symptoms, so additional examinations are necessary to make an accurate diagnosis.
The development of the disease from the first symptoms to the receipt of a doctor’s conclusion goes through the following stages:
- A condition of prethrombosis , in which people often do not go to the doctor. The patient's vision is practically unimpaired, with only periodic blurring or decreased sharpness possible. During an instrumental examination during this period, visual acuity can be recorded within 0.6-1.0, and also reveal a slight dilation of the veins and their tortuous structure. The results of ophthalmoscopy show minor hemorrhages and slight swelling.
- In the absence of adequate treatment, thrombosis of the central retinal vein develops . The patient experiences a veil before the eyes, a decrease in visual acuity to 0.2-0.6 and minor painful sensations. An ophthalmoscopic examination reveals unclear boundaries of the optic disc, tense and dilated veins, edema and exudative deposits.
After identifying central vein thrombosis, the condition of the branches and the presence of blood clots in smaller vessels are determined. The consequence of blockage may be ischemia of the affected area, which also has important diagnostic significance.
With non-ischemic thrombosis, the prognosis for the patient is more favorable. At this stage, the doctor must examine the patient’s visual system in detail to confirm the diagnosis and determine the type of thrombosis.
For this purpose, ophthalmoscopy and fluorescein angiography of the fundus are used.
- The last stage is postthrombotic retinopathy, which can develop within a few months after the circulatory disorder. At this stage, ophthalmoscopy detects hemorrhages, aneurysms, edema and other pathologies.
At this stage, the doctor must make a differential diagnosis and exclude vision pathologies caused by diabetes mellitus and other non-ophthalmological causes.
Classification
Thrombosis of branched vessels or central retinal vein is classified according to the following criteria:
- localization - the thrombus is located in the central vein or its branches;
- etiology – inflammatory or other;
- stage – prethrombosis, thrombosis, postthrombotic retinopathy, recurrent thrombus formation;
- type – non-ischemic pathology or ischemic;
- condition of the macula - edematous or not.
According to the international classification (ICD 10), this disease is listed under code H 34.8.
Etiology and pathogenesis
The formation of a blood clot in the vessels of the eye can occur for various reasons. The main provoking factors can be divided into:
- systemic – atherosclerosis, increased blood pressure, diabetes mellitus, previous infectious diseases;
- local – inflammatory processes in the retina, age-related changes in the organs of vision, glaucoma.
After the action of a provoking factor in the retinal vein system, blood flow slows down and an inflammatory process occurs. This leads to blood thickening and the formation of blood clots.
Symptoms
Symptoms of retinal vessel thrombosis may be similar to other diseases of the visual system. To make an accurate diagnosis, a more detailed examination of the patient using instrumental methods will be required.
Clinical signs depend on the stage of development of the pathology:
- Prethrombosis . This is the stage at which structural changes are already occurring, but are still poorly felt by the patient. There are no specific complaints, and the diagnosis is often made during a random eye examination. The field of vision and acuity are practically unchanged.
- Thrombosis. The patient experiences an unpleasant haze before his eyes and visual acuity noticeably decreases. The quality of life deteriorates and forces you to see a doctor. An ophthalmoscopic examination reveals hemorrhages and structural changes in the veins.
- If the blood clot affects a branch of the central vein , the patient begins to see objects distorted, and his vision deteriorates gradually over several months.
- Chronic blockage of blood vessels leads to changes in retinal trophism and retinopathy. When examining the fundus, areas of hemorrhage, macular edema, and aneurysms are revealed. In the presence of ischemia, edema is more pronounced, and hemorrhages are detected mainly in the posterior pole of the eye.
Establishing diagnosis
Assuming thrombosis of the central retinal vein, the doctor will ask the patient about the patient’s medical history, lifestyle, and also prescribe an ophthalmoscopic examination. Based on its results, making a diagnosis will not be difficult. Additionally, fluorescein angiography may be prescribed.
General principles of treatment
Treatment of central retinal vein thrombosis is aimed at:
- restoration of blood flow in the affected area;
- decreased pressure in the affected vein;
- restoration of metabolic processes and tissue nutrition;
- eliminating the root cause;
- prevention of complications.
In most cases, surgical treatment with laser is recommended. In parallel with this, maintenance drug therapy can be carried out.
- At the prethrombosis stage, anti-inflammatory drugs , anticoagulants, and artificial tear preparations are prescribed.
- At the thrombosis stage, diuretics, enzyme preparations , vitamins and anti-inflammatory drugs are used. If ischemia is observed in the affected area, laser coagulation and ultraviolet irradiation may be used.
- For retinopathy, peripheral vasodilators and anti-inflammatory drugs are prescribed.
The disease is progressive in nature, so it is not possible to talk about a successful outcome of conservative treatment. Doctors often recommend laser surgery. The earlier therapy is started, the better the result can be expected.
To receive quality medical care, it is better to be treated in a specialized ophthalmology clinic. There, the patient will undergo a complete diagnosis, determine the degree of neglect of the pathology, and prescribe the correct treatment regimen.
Complications and side effects of treatment
Modern treatment methods, such as laser coagulation, are highly effective and rarely lead to complications. In some cases, the patient may experience allergic reactions to concomitant medications, form a cyst after surgery, or develop macular edema.
Errors and unreasonable assignments
Symptoms of retinal thrombosis are similar to complications of other diseases, such as diabetes. If the patient is not fully diagnosed, the doctor may mistakenly assume a different diagnosis, taking into account some features of the medical history. In this case, unreasonable prescriptions may be made, which will lead to the progression of the pathology and a worsening prognosis.
Forecast
With early diagnosis and uncomplicated course, the prognosis is favorable. With medication it is possible to stop the progression of the pathology and achieve resorption of the blood clot. In other cases, thrombosis of the central retinal vein leads to complications, including optic nerve atrophy, glaucoma and others.
Vascular diseases occupy a leading place in the world in terms of prevalence. Problems can occur in any part of the body and always involve dysfunction of the affected organ. Find out from our other articles recommendations for varicose veins of the legs, as well as how to remove veins on the legs without surgery
Source: https://varikoza.guru/tromboz/tsentralnoj-veny-setchatki.html