Atropine eye drops are used in ophthalmology for medicinal dilation of the pupil (mydriasis) for further vision diagnostics and operations.
The effect of the medicine occurs 30-40 minutes after use and lasts about 4 days, after which the functions of the visual organs are gradually restored.
Treatment with the drug is possible only in a specialized medical institution, under the control of intraocular pressure due to possible side effects. These include photophobia, conjunctival redness, headache, dizziness, dry mouth, increased heart rate and anxiety.
Despite the low cost (from 20 to 150 rubles), the medicine is prescribed in rare cases. Instead, its safer analogues are used.
More information about the drug can be found here
When using Atropine and its analogues, it is necessary to temporarily refrain from driving vehicles and other activities that require concentration and quick reaction. It is also undesirable to wear lenses during the diagnosis and treatment of eye diseases.
Cheap analogues
These include Tropicamide drops.
Tropicamide
The drug is used for diagnosis (determining refraction, performing ophthalmoscopy) and complex treatment of eye inflammation.
It is produced under several trade names: Tropicamide, Tropicam, Midriacil. Dispensed strictly according to prescription. Its cost varies from 50 to 400 rubles. depending on the manufacturer.
Eye drops cannot be used if you are allergic to the components, intraocular hypertension and glaucoma. When using the drug, side effects may occur: increased pressure inside the eye, tachycardia, the appearance of convulsions and dry mouth, decreased visual acuity and photophobia, and undesirable mental reactions.
The incidence of undesirable effects increases with simultaneous use of antidepressants and antiallergic drugs.
The active ingredient tropicamide is included in the combination drops Midrimax and Appamide Plus, the cost of which is 600-700 rubles.
They are prescribed for diagnosing diseases of the organs of vision and during surgical and laser operations. The drug is contraindicated in children and the elderly, pregnant women, and in certain diseases - glaucoma, arrhythmia, hypertensive crisis, type 1 diabetes mellitus.
Pharmacological effects of atropine
Home Favorites Random article Educational New additions Feedback FAQ⇐ PreviousPage 5 of 17Next ⇒
1) Dilation of the pupils of the eyes (mydriasis).
Atropine eliminates the stimulating effect of parasympathetic innervation on the orbicularis iris muscle (M3-cholinoreceptor block) - the orbicularis iris muscle relaxes, contraction of the radial iris muscle predominates - the pupil dilates.
Due to the dilation of the pupils, atropine can increase intraocular pressure and is strictly contraindicated for glaucoma!
2) Paralysis of accommodation (cycloplegia).
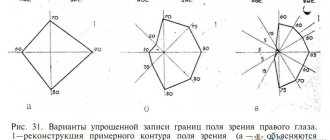
Atropine eliminates the stimulating effect of parasympathetic innervation on the ciliary (ciliary) muscle (block of M3 cholinergic receptors) - the ciliary muscle relaxes; the cinnova ligament (ciliary band) is stretched, the lens stretches in all directions and becomes flatter; The refractive power of the lens decreases, the eye is set to the far point of vision (near objects seem blurry); characterized by micropsia (seeing objects in a reduced size).
3) Increased heart rate (tachycardia).
Atropine eliminates the inhibitory effect of parasympathetic innervation (vagus) on the sinoatrial node (M2-cholinergic receptor block); The automaticity of the sinoatrial node increases - heart contractions become more frequent. Due to the fact that atropine stimulates the vagal centers, tachycardia may be preceded by bradycardia.
4) Facilitation of atrioventricular conduction.
Atropine eliminates the inhibitory effect of parasympathetic innervation (vagus) on the atrioventricular node (M2-cholinergic receptor block); conduction of the atrioventricular node is facilitated.
5) Relaxation of smooth muscles of the bronchi, gastrointestinal tract, bladder.
Atropine eliminates the stimulating effect of parasympathetic innervation on the smooth muscles of the bronchi, stomach, intestines, bladder (block of M3 cholinergic receptors) - relaxation of the smooth muscles of these organs occurs.
6) Decreased secretion of bronchial and digestive glands.
Atropine eliminates the stimulating effect of the parasympathetic
innervation to the glands (block of M3 cholinergic receptors) - the secretion of the bronchial glands, salivary glands, gastric glands, and pancreas decreases.
7) Decreased secretion of sweat glands.
Atropine blocks the stimulating effect of atypical (cholinergic) sympathetic innervation on the sweat glands (block of M3 cholinergic receptors) - sweating decreases.
In addition, atropine blocks M3 cholinergic receptors in the endothelium of blood vessels. Since most of the blood vessels do not receive cholinergic innervation, the M3-cholinergic receptors of the vessels are non-innervated and when they are blocked by atropine, the tone of the blood vessels does not change. At the same time, atropine eliminates the vasodilatory effect of substances that stimulate M3 cholinergic receptors (Fig. 14).
Use of atropine
1. Ophthalmology.
Atropine is used for iritis and iridocyclitis, since dilation of the pupils reduces the possibility of the formation of inflammatory adhesions between the iris and the lens capsule.
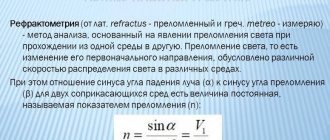
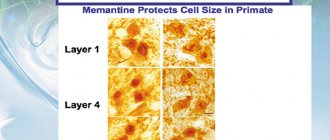
Atropine can be used to examine the fundus of the eye (dilation of the pupils) or to determine the true refraction of the eye (determining the refractive power of the lens in case of paralysis of accommodation). However, the duration of action of atropine on the eye is about 7 days, so for these purposes shorter-acting M-anticholinergics are used, for example, tropicamide (effective for about 4 hours).
2. Cardiology.
Atropine is used for bradyarrhythmias and atrioventricular block.
3. Pulmonology.
Atropine is used for bronchial asthma.
4. Gastroenterology.
Atropine is used for gastric and duodenal ulcers, as well as for hyperacid gastritis; The ability of atropine to reduce the secretion of hydrochloric acid and eliminate painful spasms of the stomach and duodenum is used.
Atropine
—
Atropine reduces the secretion of HC1, as it blocks: - M3-cholinergic receptors of parietal cells (production of HC1 decreases);
- M1-cholinergic receptors of enterochromaffin-like cells (the release of histamine, which stimulates parietal cells, decreases);
- M3-cholinergic receptors of G-cells that secrete gastrin (the production of gastrin, which stimulates enterochromaffin-like cells, decreases);
— M2-cholinergic receptors of D-cells of the stomach, producing somatostatin (with blockade of M2-cholinergic receptors, the release of somatostatin increases; somatostatin reduces the activity of enterochromaffin-like cells; Fig. 51.
Atropine is effective for intestinal colic (painful intestinal spasms), less effective for hepatic colic, and ineffective for renal colic.
5. Anesthesiology.
Atropine is used as premedication during surgical operations to prevent reflex bradycardia, as well as to reduce excessive secretion of the salivary and bronchial glands.
Side effects of atropine: dry mouth, photophobia (fear of bright light), impaired near vision, tachycardia, constipation, difficulty urinating.
Atropine poisoning is characterized by: mental and motor agitation, dilated pupils, impaired near vision, hoarse voice, difficulty swallowing, tachycardia, dryness and redness of the skin (due to impaired heat transfer, an increase in temperature is possible, especially in children), impaired urination (urinary catheterization is required). bubble).
With more severe poisoning, motor and mental agitation increases with confusion. Patients lose orientation, stop recognizing others, they develop visual and auditory hallucinations, and delusions. In very severe cases, convulsions occur, which are replaced by a state of depression, coma. Death occurs from paralysis of the respiratory center.
Atropine has a high affinity for M-cholinoreceptors. Therefore, M-cholinomimetics are little effective in atropine poisoning. Physostigmine, a solution of which is administered intramuscularly, has some therapeutic effect. The rest of the treatment is symptomatic. When taking atropine orally, it is necessary to lavage the stomach through a tube with the introduction of activated carbon, 0.05% potassium permanganate solution or tannin solution (you can use strong tea). To reduce agitation, diazepam is administered intravenously. If necessary, perform artificial ventilation. To remove poison from the blood, hemosorption and forced diuresis are used.
Among medicines containing atropine, in some cases belladonna (belladonna) preparations - tincture and extracts (dry and thick). These drugs are prescribed orally most often for pain associated with spasms of smooth muscles of the gastrointestinal tract, bile ducts (cholecystitis, cholelithiasis). Belladonna extracts are also prescribed in rectal suppositories.
Scopolamine is an alkaloid found in the same plants as atropine; its highest content is in scopolia. The chemical structure and pharmacological properties of scopolamine are similar to atropine. Unlike atropine, scopolamine in therapeutic doses has a distinct depressant effect on the central nervous system, acting as a sedative (calming) agent.
In practical medicine, the inhibitory effect of scopolamine on the vestibular apparatus is used. Scopolamine is used for vestibular disorders (dizziness, imbalance, gait problems), and for the prevention of motion sickness (sea and air sickness). Scopolamine is part of Aeron tablets, which are taken before sea trips or airplane flights. The duration of action of these tablets is about 6 hours. For long trips, a transdermal therapeutic system with scopolamine is used - a patch that releases scopolamine for 72 hours; The patch is applied to healthy skin behind the ear.
In addition, scopolamine is used in the same cases as atropine: before anesthesia to prevent reflex bradycardia and reduce the secretion of the salivary and bronchial glands, and also as an antispasmodic.
Tropicamide is used in ophthalmological practice in eye drops to examine the fundus and determine the true refraction of the eyes. Mydriasis and cycloplegia develop within 20-30 minutes. Duration of action is 2-4 hours.
In ophthalmic practice, homatropine and cyclopentolate are also used, which act for about 24 hours.
Ipratropium (Atrovent) is used in the form of an aerosol for bronchial asthma.
Platyphylline is a ragwort alkaloid. In addition to M-anticholinergic activity, platiphylline has a myotropic antispasmodic effect, i.e. relaxing effect directly on the smooth muscles of internal organs and blood vessels. Thus, the ability of platyphylline to relax the smooth muscles of internal organs is due to M-anticholinergic activity and myotropic antispasmodic properties.
Due to the myotropic antispasmodic effect, platiphylline, unlike other M-cholinergic blockers, dilates blood vessels and can slightly reduce blood pressure.
Platiphylline is used (prescribed orally or injected under the skin) mainly for spasms of smooth muscles of the abdominal organs, gastric and duodenal ulcers, and bronchial asthma.
Pirenzepine (gastrocepin) blocks predominantly M1-cholinergic receptors. Due to the blockade of M1-cholinergic receptors of enterochromaffin-like cells, pirenzepine reduces their ability to release histamine. Due to a decrease in histamine production, the secretion of hydrochloric acid from gastric juice by parietal cells decreases.
In average therapeutic doses, pirenzepine has little effect on pupil size, accommodation, heart contractions and only causes some dry mouth. Used in the treatment of peptic ulcers.
Trihexyphenidyl (cyclodol) has a pronounced inhibitory effect on M-cholinergic receptors of the central nervous system. Used for Parkinson's disease.
Darifenacin selectively blocks M3 cholinergic receptors; can be used clinically to reduce bladder tone.
All M-anticholinergic drugs are contraindicated for glaucoma!
Ganglioblockers
Ganglion blockers block NN-cholinergic receptors of neurons of the sympathetic and parasympathetic ganglia, chromaffin cells of the adrenal medulla, and carotid glomeruli. Thus, ganglion blockers block sympathetic and parasympathetic innervation equally at the ganglion level. Against the background of the action of ganglion blockers, M-cholinomimetics and adrenergic mimetics cause the usual effects.
Ganglion blockers reduce the secretion of adrenaline and noradrenaline by the adrenal glands and prevent reflex excitation of the respiratory and vasomotor centers from the NN-cholinergic receptors of the carotid glomeruli. Ganglion blockers that penetrate the blood-brain barrier (for example, mecamylamine) block NN-cholinergic receptors of the central nervous system.
Ganglionic blockers act as antagonists of NN-cholinoreceptors of the autonomic ganglia. Their action is manifested in eliminating the influences of sympathetic and parasympathetic innervation. The greater the influence of a particular innervation, the greater the blocking effect.
Thus, parasympathetic innervation has a more pronounced influence on the size of the pupils: the pupils are usually somewhat constricted (contraction of the circular muscle of the iris). In this case, the blocking effect of ganglion blockers on parasympathetic innervation will be more pronounced - ganglion blockers cause dilation of the pupils (mydriasis).
The ciliary muscle receives mainly parasympathetic innervation. Ganglion blockers, by blocking the parasympathetic ganglia, cause relaxation of the ciliary muscle - paralysis of accommodation.
The heart rate is 70% determined by the inhibitory effect of the vagus. Ganglion blockers eliminate the inhibitory effect of the vagus on the sinoatrial node and usually cause tachycardia.
The strength of contractions of the ventricles of the heart is determined by the influences of sympathetic innervation (parasympathetic innervation of the ventricles is poor). Ganglion blockers eliminate the stimulating effect of sympathetic innervation and weaken heart contractions. The stroke output of the heart decreases. Despite the tachycardia, the cardiac output also decreases somewhat.
The vagus has an inhibitory effect on atrioventricular conduction, and sympathetic innervation has an activating effect. Normally, these influences are balanced. Therefore, ganglion blockers do not have a significant effect on atrioventricular conduction.
Most blood vessels (arteries and veins) receive only sympathetic innervation. Ganglion blockers eliminate the stimulating effect of sympathetic innervation and cause dilation of arterial and venous vessels - arterial and venous pressure decreases. Blood pressure also decreases due to a decrease in cardiac output. A decrease in blood pressure is facilitated by the blockade of NN-cholinergic receptors of chromaffin cells of the adrenal medulla by ganglion blockers and a decrease in the production of adrenaline and norepinephrine.
The smooth muscles of the bronchi receive only parasympathetic innervation, which has a bronchoconstrictor effect.
At the same time, in the smooth muscles of the bronchi there are non-innervated β2-adrenergic receptors, which are excited by adrenaline (brochodilator effect). Normally, these influences are balanced. Therefore, ganglion blockers usually do not have a significant effect on bronchial tone.
Contractions of the smooth muscles of the gastrointestinal tract and bladder (with the exception of sphincters), as well as the secretion of the salivary, bronchial glands, glands of the stomach and intestines are determined by the stimulating influence of parasympathetic innervation. Ganglion blockers reduce the peristalsis of the gastrointestinal tract, the tone of the bladder, and the secretion of the bronchial and digestive glands.
Ganglion blockers reduce the secretion of sweat glands (block of atypical sympathetic cholinergic innervation).
In medical practice, the hypotensive effect of ganglion blockers is mainly used. For hypertensive crises, hexamethonium benzosulfonate (benzohexonium) or azamethonium (pentamine) is administered subcutaneously or intramuscularly. The effect of these drugs lasts 2-3 hours.
The ultra-short-acting ganglion blocker trimetaphan (arfonad) acts for 10-15 minutes. Solutions of the drug are administered intravenously for controlled hypotension (lowering blood pressure for the required time during surgical operations, for example, to reduce blood loss, prevent cerebral edema).
Mecamylamine (mecamine) is a non-polar compound (secondary amine); unlike hexamethonium, azamethonium (quaternary ammonium compounds) and trimethaphane (sulfonium compound) easily penetrates the central nervous system and blocks central NN-cholinergic receptors. In this regard, mecamylamine reduces the euphoric effect of nicotine and can be used to quit smoking.
Side effects of ganglion blockers: mydriasis, paralysis of accommodation, dry mouth, nasal congestion, decreased intestinal motility and bladder tone, severe orthostatic hypotension (a sharp drop in blood pressure when moving from a horizontal to a vertical position). Due to the possibility of orthostatic hypotension, patients are recommended to lie in bed for at least 1.5-2 hours after administration of a ganglion blocker.
⇐ Previous5Next ⇒
Recommended analogues
The safest analogues of Atropine are the drugs Irifrin and Irifrin BC.
Irifrin
Drops are used to dilate the pupil. Additionally, they eliminate red eye syndrome and constrict the vessels of the conjunctiva. If the dosage is observed, the medicine does not affect the psyche and does not cause anxiety.
Irifrin is most convenient for diagnostic purposes: it dilates the pupil after a single instillation after 15-30 minutes. The effect lasts up to 3 hours, which does not cause additional inconvenience to the patient.
Drops can be used in children from 6 years of age as prescribed by a doctor.
Possible side effects: burning sensation and discomfort, increased intraocular pressure, tachycardia, arrhythmia.
The cost of the drug in different pharmacies varies from 550 to 650 rubles.
Irifrin BK
The price of the medicine is slightly higher (650-700 rubles), since it does not contain preservatives and is available in disposable droppers. This allows them to be used by people allergic to preservatives.
Also, the use of disposable droppers is convenient during a long course of treatment: the bottle with drops itself does not serve as a source for the growth of bacteria and less often leads to the occurrence of bacterial and viral conjunctivitis.
Author's rating
Author of the article
Alexandrova O.M.
Articles written
2031
about the author
Was the article helpful?
Rate the material on a five-point scale!
( 4 ratings, average: 5.00 out of 5)
If you have any questions or want to share your opinion or experience, write a comment below.