Endophthalmitis is called abscess inflammation in the internal structures of the eye, which leads to the accumulation of purulent exudate in the vitreous body. The disease is manifested by pain in the eyeball, swelling, redness of the conjunctiva and eyelids, a significant drop in visual acuity, as well as hypopyon.
Purulent inflammation of the eye tissues are among the most dangerous ophthalmological conditions that require emergency specialized care. The course of the purulent process with endophthalmitis is rapid. Sometimes, in just a few hours, it can lead to the development of panophthalmitis - a state of total inflammation with melting of all the membranes of the eye, including orbital tissue. According to various sources, the incidence of blindness and eye death, which leads to enucleation, in patients with intraocular infection ranges from 28 to 89%. Such circumstances make it necessary for timely prevention, early detection and selection of adequate treatment for eye infections.
Causes
A dangerous disease in which the eye turns red and vision deteriorates, occurs due to the influence of various factors - this is endophthalmitis. Quite often, the infection is spread by microbes that enter the membrane of the visual organ along with a foreign object. Lead to inflammation:
- Chemical burns.
- Penetrating wounds.
- Operations and interventions.
- Complications of corneal ulcers.
The eyes of people who suffer from tonsillitis and osteomyelitis are affected. Pathology can begin with blood poisoning or inflammation of the paranasal sinuses. Its causative agents are candida fungi and neurospora, bacteria such as:
- Klebsiella;
- Pseudomonas aeruginosa;
- Proteus;
- streptococci.
A purulent process is formed if the connective tissue is affected, and boils form on the body. Joint diseases, immunodeficiency, and advanced caries can provoke inflammation.
A serious disease that affects the posterior part of the choroid of the visual organ is chorioretinitis of the eye.
Klebsiella is a type of bacteria that can cause a dangerous illness.
The causes of central serous chorioretinopathy are described here.
Causes
In most cases, panophthalmitis develops 2-3 days after a penetrating eye injury.
It is also possible to develop due to hematogenous penetration of infection into the tissue of the eyeball, usually due to sepsis. Less often - due to infectious diseases of another localization. May develop as a complication of other ophthalmological diseases of bacterial etiology:
- keratitis;
- corneal ulcers;
- uveitis;
- endophthalmitis;
- phlegmon of the orbit;
- abscess formation of the eyelid.
Postoperative occurrence of panophthalmitis is possible (prolonged intervention, improper asepsis, poor care in the postoperative period). Cases of total purulent eye lesions have been recorded against the background of:
- tuberculosis;
- pneumonia;
- meningitis;
- furunculosis;
- sinusitis.
The main causative agents of panophthalmitis, like most other bacterial diseases, are Escherichia coli or Pseudomonas aeruginosa, cocci (streptococci, pneumococci, staphylococci), and Mycobacterium tuberculosis.
Why does endophthalmitis occur?
Endophthalmitis occurs for reasons of external and internal nature. In the first case it is:
- Mechanical damage (95% of identified cases of the disease).
- Previous operations on the visual organs.
- Breakthrough of an ulcer with pus located on the cornea.
- Chemical burns to the eyes.
- Contact with foreign objects in the eyes.
Internal factors for the formation of endophthalmitis are based on infection of the visual organs by pathogenic organisms. In addition, the infection can be transferred to the eyes from other tissues of the body in diseases such as meningitis, tonsillitis, sinusitis, and sepsis. Fungi also lead to the development of the disease.
Classification
Depending on which cavities of the eye are involved in the purulent process, a focal form of pathology is distinguished, when the abscess is present only in the vitreous body.
With diffuse endophthalmitis, the adjacent tissues and bones of the orbit become inflamed. In the mixed form, different membranes of the visual organ are affected, the purulent process develops only in several or even in one focus.
With a mild degree of pathology, the eyelid swells and the eye turns red, but this does not prevent the person from viewing objects normally. In the moderate form, hyperemia intensifies, vision decreases, and pain appears. It becomes unbearable with severe endophthalmitis, when pus begins to secrete and the eye swells greatly. The patient sees practically nothing.
The traumatic form of pathology occurs when the membrane of the visual organ is damaged if it gets infected. With fungal endophthalmitis, which is caused by neurospora, candida, and aspergillus, the symptoms are mild. Purulent pathology develops when bacteria that enter the visual organ are activated.
The phacoanaphylactic form of endophthalmitis occurs when, after surgery or injury, the lens ruptures, protein enters the vitreous, and autoimmune inflammation begins.
An effective mydriatic remedy is Cyclomed eye drops.
Aspergillus is a dangerous fungus that causes serious diseases of the respiratory tract and visual organs
The pathology quickly spreads and invades other structures of the visual organ, and the membranes melt. It turns into panophthalmitis, which is accompanied by:
- abnormal lacrimation;
- photophobia;
- chemosis of the conjunctiva;
- fever or chills;
- blepharospasm.
After a penetrating wound or severe trauma, the eye becomes inflamed within two days. The iris melts, the cornea loses its transparency, and the vitreous body fills with pus. A person stops perceiving light, begins to see objects poorly, and may even go blind.
With panophthalmitis, blepharospasm often develops
Is it worth saving and using an inexpensive analogue instead of the original remedy when it comes to mydriasis - cyclopentolate eye drops.
Clinical picture
Chemosis and hyperemia of the eyeball and a clouded iris pattern are characteristic. During an ophthalmological examination, purulent discharge can be seen in the bottom of the anterior chamber of the eye. After 1-3 days, pus fills the entire anterior chamber of the eyeball, which causes blindness. The mobility of the eyeball is sharply limited and painful. In this case, the pain radiates to the temporal region, frontal lobes and the back of the head.
In the absence of treatment, the cornea and sclera are involved in the purulent process: the tissues melt, forming a single purulent mass. The lesion then spreads to the prebulbar tissues and Tenon's capsule, which leads to complete atrophy of the muscles and ligaments.
Prevention
The main route of infection of the vitreous body is traumatic injuries and foreign bodies
. Therefore, the most effective measure for preventing endophthalmitis is the prevention of injury.
For any damage, especially when injured by a foreign body, complete primary surgical treatment of the wound is necessary in the coming hours after the incident. All foreign matter must be removed and the wound carefully treated.
To prevent wound infection, antibiotics are prescribed, systemically and locally in the form of solutions, gels or ointments. Patients with deep damage to the eyeball may be offered hospitalization.
Panophthalmitis
- Etiology
- Clinical picture
- Diagnosis of panophthalmitis
- Treatment
Panophthalmitis is an acute purulent inflammation of all tissues and membranes of the eye. Panophthalmitis is the extreme and most severe form of inflammation of the organ of vision, in which all the membranes of the eye and surrounding soft tissues (eyelids, tissue, muscles) are involved in the purulent process. The seriousness of the problem lies in the fact that panophthalmitis often leads to death and subsequent atrophy of the eye. Protective mechanisms are concentrated in the appendage apparatus of the eye (eyelids, lacrimal glands), so the penetration of infection into the eyeball is accompanied by rapid and unhindered proliferation of microorganisms. As a result, with panophthalmitis, all layers of the eyeball are exposed to purulent inflammation and melting.
Etiology
Panophthalmitis can be caused by exogenous or endogenous penetration of infection into the eyeball. In this case, the causative agents are usually streptococci, staphylococci, pneumococci, Pseudomonas aeruginosa and Escherichia coli, and Mycobacterium tuberculosis. In ophthalmology, panophthalmitis is most often caused by penetrating injuries of the eye (mechanical damage, foreign bodies, burns). In this case, a purulent infection penetrates deep into the eyeball through the wound canal. Panophthalmitis can also be a consequence of bacterial keratitis, perforation of a purulent corneal ulcer, severe uveitis, blenorrhea, trachoma, eyelid abscess, orbital phlegmon, endophthalmitis. Endogenous infection of eye structures is less common and may be associated with metastatic introduction of bacterial infection from distant purulent foci. The occurrence of panophthalmitis is possible due to pneumonia, tuberculosis, furunculosis, postoperative or postpartum sepsis, meningitis, typhus, sinusitis.
Clinical picture
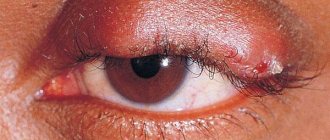
With penetrating wounds of the eyeball, panophthalmitis develops rapidly, within 2-3 days. Purulent damage to the structures of the eye is accompanied by severe pain in the eyeball, lacrimation, photophobia, reflex blepharospasm, and a rapid and significant decrease in vision.
Objective changes are characterized by severe hyperemia, swelling of the conjunctiva and eyelids, which can lead to chemosis - pinching of the eye mucosa by the eyelids. The cornea becomes cloudy and swollen, the iris melts, pus accumulates in the anterior chamber of the eye, purulent exudate is also found in the vitreous body. With panophthalmitis, there is a rapid and significant decrease in vision up to light perception or blindness. With further progression of panophthalmitis, pus penetrates under the conjunctiva, infiltrates the peribulbar tissues, spreads into Tenon's capsule, increasing tissue swelling and leading to the development of inflammatory exophthalmos. The mobility of the eyeball is sharply limited. Perforation of the sclera may occur with the release of pus to the outside. Subsequently, after 6-8 weeks, the eye shrinks and atrophies.
With anaerobic panophthalmitis, the purulent process develops rapidly: a coffee-colored discharge with gas bubbles appears from the anterior chamber, blindness occurs already on the day the eye is injured. In addition to local changes, panophthalmitis is accompanied by general symptoms: intoxication, headache, fever with chills, vomiting. The purulent process can spread to the meninges with the development of meningitis and the formation of a brain abscess.
Diagnosis of panophthalmitis
For the diagnosis of panfotalmitis, the presence of a history of penetrating wounds of the eye and infectious foci in the body is of paramount importance. Objective signs of panophthalmitis (changes in the conjunctiva, iris, accumulation of purulent exudate in the anterior chamber of the eye and the vitreous body) are detected by an ophthalmologist when examining the structures of the eye (diaphanoscopy, biomicroscopy). If it is possible to examine the fundus using ophthalmoscopy, dilated retinal veins are determined. Ultrasound scanning allows you to identify foci of destruction of the deep structures of the eye.
To determine the microbial flora that caused the development of panophthalmitis, corneal paracentesis is performed to obtain purulent exudate and its bacteriological culture. Differential diagnosis of panophthalmitis is carried out with endophthalmitis, which is not so violent.
Treatment
Panophthalmitis requires early and intensive treatment. The basis of pathogenetic therapy for panophthalmitis is the administration of massive doses of antibiotics (benzylpenicillin, streptomycin, monomycin, gentamicin, etc.). Antibiotics are administered intramuscularly, intravenously, in the form of retrobulbar, subconjunctival injections. In some cases, vitrectomy and intravitreal administration of antimicrobial agents are resorted to. Instillations and baths with trypsin solution are indicated. To eliminate the phenomena of general intoxication, intravenous infusions of saline solutions are performed.
Conservative treatment of panophthalmitis is not always successful, so it is often necessary to resort to evisceration or enucleation of the eyeball, followed by ocular prosthetics.
With timely initiation of complex treatment of panophthalmitis, in some cases it is possible to preserve the eyeball and residual vision. The most common outcome of panophthalmitis is the death of the eye with its subsequent atrophy. The prognosis for visual function and life with panophthalmitis is always extremely serious. The main role in the prevention of panophthalmitis belongs to the prevention of eye injuries, sanitation of infectious foci in the body, treatment of inflammation of the structures of the eye and its adnexal apparatus. In case of eye injuries, it is necessary to carry out preventive local and general antibiotic therapy in the first hours after the injury.
Signs of a purulent process
The main symptom of inflammation that occurs in the tissues of the visual organ is pain in the eye, radiating to the head. With endophthalmitis, the upper eyelid turns red and swells, fibrous fluid accumulates on the iris, which looks like a yellow stripe. The purulent process is accompanied by:
- increase in intraocular pressure;
- severe lacrimation;
- the appearance of a blurry picture;
- blurred vision.
Scars form, causing the eyeball to become deformed. A yellowish spot becomes noticeable in the pupil, color perception is impaired, and vision decreases.
Blurred vision is one of the first symptoms of the disease
A product that has an antimicrobial, astringent, drying and local anti-inflammatory effect - boron zinc eye drops.
Causes of panophthalmitis
The eye is well protected from infections, but the protective mechanisms are located in the adnexa of the eye - the eyelids and lacrimal glands. If the infection penetrates the cavity of the eyeball, rapid proliferation of pathogenic bacteria begins. Most often, panophthalmitis is caused by staphylococci, streptococci, pneumococci, mycobacterium tuberculosis, Escherichia coli and Pseudomonas aeruginosa.
Pathogens of purulent inflammation can enter the eyeball from the outside (exogenous infection) or from other parts of the body (endogenous infection). The cause of panophthalmitis of exogenous etiology is most often penetrating wounds of the eyeball, when the infection enters the eye through the wound canal. In addition, panophthalmitis can develop due to perforation of a purulent ulcer on the cornea, with severe bacterial uveitis or keratitis.
Endogenous inflammation of the eye is much less common; in this case, metastatic introduction of pathogens of the purulent process from distant foci occurs (this is possible with furunculosis, tuberculosis, meningitis and some other diseases).
Preventive measures
Unfortunately, like any eye disease, this pathology is characterized by serious complications. The reason for this result is diagnostic errors, neglected processes and incorrect therapy. If a failure occurs at any stage, the patient risks getting:
- complete blindness without the possibility of recovery;
- functional as well as anatomical death of the eye, which often ends with the removal of the apple and installation of a prosthesis;
- subatrophy and atrophy of the eyeball;
- panophthalmitis.
For this reason, there is no need to start the disease. In any city you can find an ophthalmology department similar to the Helmholtz Clinic, and there you can receive qualified assistance from a group of doctors.
To avoid the occurrence of endophthalmitis, precautions must be taken. For example, to prevent possible eye injuries. In a situation where an injury occurs, first aid should be provided with proper treatment of the wound.
If a person has a foreign body in the eye, it must be removed immediately. Sometimes it is impossible to do this on your own, then you should contact an ophthalmologist on duty.
Sanitation of purulent areas must be done in a timely manner, and not wait for it to spread to neighboring areas. Doctors suggest therapy for this condition. Ophthalmologists give favorable prognoses if treatment was started on time, then it is possible to preserve the eyeball, avoid blindness and reduce the risk of possible relapses.
Forecast and prevention of panophthalmitis
With timely initiation of complex treatment of panophthalmitis, in some cases it is possible to preserve the eyeball and residual vision. The most common outcome of panophthalmitis is the death of the eye with its subsequent atrophy. The prognosis for visual function and life with panophthalmitis is always extremely serious.
The main role in the prevention of panophthalmitis belongs to the prevention of eye injuries, sanitation of infectious foci in the body, treatment of inflammation of the structures of the eye and its adnexal apparatus. In case of eye injuries, it is necessary to carry out preventive local and general antibiotic therapy in the first hours after the injury.
Panophthalmitis is a total purulent inflammation of the eyeball, accompanied by melting of all its structures and membranes. Panophthalmitis develops with the occurrence of sharp pain in the orbit and head on the affected side, lacrimation, photophobia, swelling and chemosis of the conjunctiva, blepharospasm, chills, fever and loss of vision. To diagnose panophthalmitis, the following studies are used: diaphanoscopy, biomicroscopy, ophthalmoscopy, ultrasound of the eye, bacteriological culture. Treatment of the disease requires timely active local as well as systemic antibacterial therapy. In some cases - evisceration or enucleation of the eye.
Panophthalmitis is an extremely severe form of inflammation of the organ of vision, with the involvement of all membranes of the eye and surrounding soft tissues (eyelids, muscles, fiber) in the purulent process. The seriousness of the problem is that the disease often leads to the death of the eye. The protective mechanisms of the organ of vision are concentrated in its appendage apparatus (eyelids and lacrimal glands), so infectious agents penetrating inside have the opportunity to multiply rapidly and unhindered. As a result, all areas of the eyeball are subject to purulent inflammation and further melting.
Diagnostics
To identify the presence of endophthalmitis, interviewing the patient, measuring intraocular pressure and anamnesis are not enough. The ophthalmologist conducts a number of instrumental examinations.
Biomicroscopy using a slit lamp helps to detect structural damage, infiltration of the iris, and accumulation of pus in the eye cavity.
Find out what ailments Tsipromed eye drops will help you get rid of here.
The slit lamp is indispensable for diagnostic purposes
To examine the yellowish spot in the pupil, which indicates the presence of an abscess in the vitreous, proceed to diaphanoscopy. In case of inflammation in the visual organ, diagnosis cannot be done without examination using:
- electroretinography;
- Ultrasound;
- ophthalmoscopy.
The first method, in which special equipment is used, determines both the biopotential and the condition of the retina.
With ophthalmoscopy, the fundus of the eye is checked, but this diagnostic method is only suitable for mild forms of pathology.
The article is intended for informational purposes. Only a doctor selects the method of treatment and prescribes medications, using the results of the examination. The sooner endophthalmitis is detected, the greater the chance of stopping the decline in vision and preventing the purulent process from spreading to the other eye.
To detect focal or point opacities that form in the tissues of the vitreous body, they resort to ultrasound.
Broad-spectrum antibiotic – Cipropharm eye drops.
At the initial stage, the administration of non-steroidal anti-inflammatory drugs is indicated in conjunction with injections.
Read the article about what ailments Ciprofloxacin eye drops will help you get rid of.
Diagnosis of panophthalmitis
To make a diagnosis, the first step is to find out whether there are purulent foci in the patient’s body that could provoke a complication. The fact of eye injury, foreign body entry or other mechanical damage is also important.
Important! If there is pain in the eye, redness and swelling, as well as after injury, urgent medical examination, diagnosis and surgical treatment are necessary. Even in one day you can lose your sight forever.
Objective signs of this disease are:
- Changes in the iris.
- Purulent contents in the vitreous body.
- Dilated retinal veins.
An ophthalmologist performs:
- Diaphanoscopy.
- Biomicroscopy.
- Ultrasound scanning.
- Corneal paracentesis.
- General blood analysis.
When making a diagnosis, differential diagnosis with endophthalmitis is important (this disease is not as pronounced). However, with inadequate and untimely treatment, it also very often turns into panophthalmitis.
Symptoms
Endophthalmitis manifests itself 2-4 days after injury. Includes the following symptoms:
- decreased vision;
- the appearance of purulent inflammations, which can be seen with the naked eye by a yellowish coating;
- sharp pain and general discomfort;
- corneal clouding;
- an acute reaction to light is possible, especially when moving from a dark room to a light one;
- swelling;
- redness and irritation;
- inflammation of the membrane of the eye (eyes are “bloodshot”);
- the appearance of a “veil” before the eyes, blurred vision;
The first symptoms are sharp pain and decreased visual acuity. The disease develops rapidly. Within a day, almost all the symptoms of the disease appear.
Treatment
If inflammation is detected in the vitreous body, the person is sent to the hospital. High doses of cephalosporin or penicillin antibiotics are administered intravenously, sulfonamides are prescribed, and instillations are made with drops that negatively affect pathogenic flora. The eyelids are treated with antibacterial ointments.
Corticosteroids such as prednisolone and non-steroidal anti-inflammatory drugs such as ibuprofen are used. Antihistamines are used to relieve redness and swelling.
Antibiotic injections are administered into the internal chamber and supraorbital artery. Injections of Lidaza and Trypsin help prevent the appearance of scars and fistulas.
If conservative therapy does not give a positive result, the retina exfoliates and adhesions have formed, they resort to vitrectomy. With this intervention, the vitreous body has to be removed. After surgery, antibiotic injections are repeated.
Prednisolone relieves inflammation and tissue swelling
It is important not to miss the first signs of the disease and start therapy in a timely manner - find out the possible causes of black spots before your eyes.
Symptoms of acute postoperative endophthalmitis
The symptoms and treatments for endocrine ophthalmopathy are described in detail here.
Treatment of panophthalmitis
Should begin with early intensive care. It must be comprehensive, in a hospital setting with bed rest.
The basis of treatment is the introduction of strong antibacterial drugs into the patient’s body. Antibiotics must be broad-spectrum and administered in various ways:
- intravenously;
- intramuscularly;
- subconjunctival;
- retrobulbar.
Nonsteroidal anti-inflammatory injections and infusions of saline solutions, which are necessary for severe intoxication of the body, are also important. They are administered through intravenous injections or droppers.
If conservative therapy is ineffective and complications occur extensively, surgical treatment is used. Since panophthalmitis contributes to the melting of the eyeball, mixing with purulent exudates, such a serious operation as evisceration is required to preserve the patient’s health. During this operation, several punctures (cuts) are made to completely remove the contents of the eye. Sometimes vitrectomy is performed (partial and sometimes complete removal of the vitreous). After evisceration, ocular prostheses are placed.
If the eye contents are severely damaged, we are no longer talking about saving the eye, the main thing is to save the body and prevent the development of further complications, for example, meningitis.