Sympathetic ophthalmia (from Greek - “eye susceptible to influence”) is an inflammatory lesion of a healthy eye that occurs against the background of injury or other disease of the second eye. In most cases, ophthalmia occurs in the form of anterior uveitis.
If we take into account the frequency of penetrating injuries to the organs of vision, we can conclude that the prevalence of the pathology is rather low.
Some time may pass from direct injury to the eye to the appearance of inflammation in the second eye, which is considered the latent period of sympathetic ophthalmia.
The duration of this time may vary, but most often it is 4-8 weeks from the moment of injury to the first eye (not earlier than 12 days).
Experts do not limit the maximum period for the development of the disease, since cases of signs of sympathetic ophthalmia appearing several years after injury have been recorded.
Treatment of sympathetic ophthalmia
Treatment tactics for sympathetic ophthalmia depend on the form and severity of the disease.
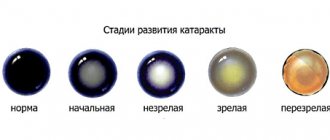
For anterior serous uveitis, local use of corticosteroids in the form of drops or parabulbar injections is indicated. The duration of the course of conservative therapy is 6 months. After treatment, relapses are usually not observed. The development of plastic uveitis is an indication for a course of local and systemic glucocorticosteroid therapy. The duration of use of glucocorticosteroids is 5-6 months. After their discontinuation, non-steroidal anti-inflammatory drugs (NSAIDs) must be taken for 3-4 weeks. The development of a generalized form of sympathetic ophthalmia requires systemic pulse therapy with corticosteroids in high dosages for 3-4 days and immunosuppressants in a standard dose. Then the dosage of the drugs is gradually reduced. The indication for discontinuation of the course of treatment is persistent remission of sympathetic ophthalmia. Surgery is indicated for the development of secondary cataracts. This involves phacoemulsification of the cataract followed by implantation of an intraocular lens. The clinical manifestations of ocular hypertension with pupil occlusion and involvement of the iris in the pathological process can be eliminated by laser membranetomy.
Prognosis and prevention of sympathetic ophthalmia
There is no specific prevention of sympathetic ophthalmia. Nonspecific preventive measures boil down to compliance with safety precautions (wearing safety glasses and a helmet) at work, prevention of viral diseases, and timely treatment of erosive damage to the organ of vision. Patients with sympathetic ophthalmia should be closely monitored by the treating ophthalmologist. Timely diagnosis and treatment ensure complete restoration of visual functions. However, in severe forms of the disease with binocular damage, there is a high risk of complete loss of vision and subsequent disability of the patient. The prognosis for life and ability to work depends on the severity of the disease and the effectiveness of the therapy.
Mysteries and subtleties of sympathetic ophthalmia
It so happened that this serious disease, known since the time of Hippocrates, began to be written about in medical scientific periodicals only in the 19th century. Sympathetic ophthalmia (SO) occurs infrequently - 1-2 cases per thousand injured eyes. Nevertheless, both among specialists and among the people, the memory of the disease is firmly “stuck”: the “transition” of inflammation to the other eye, the fear of complete blindness after damage to one eye - all this is not invented. But how is inflammation transmitted from one eye to the other? How to predict the occurrence of CO? And besides the mysteries and a lot of subtleties, there is also a paradox: frequent enucleation of the injured eye only because of the threat of rare cases of OM. Previously, such deletions were 40-50 percent, now - 5-10 percent. The numbers are very large.The scientific secretary of the Moscow Research Institute of Eye Diseases named after. Helmholtz professor Larisa Arkhipova, who has been studying this problem for more than 30 years.
From description to theory
For the first time, the clinical picture and description of 6 cases of the disease were given in 1835 by the British physician MacKenzie, who also pointed out the unfavorable prognosis and proposed the term “ophthalmia sympathica,” which is firmly established in ophthalmology. Previously, almost 70-80 percent. cases of OM led to blindness. It was only with the advent of powerful medications several decades ago that the situation began to slowly but seriously improve.
The theories of the origin of sympathetic ophthalmia have also undergone changes. If previously it was thought that after a penetrating injury to the eye, the inflammatory process spreads to the other eye along the optic or ciliary nerves, that some unidentified microbe or virus is to blame, now the autoimmune nature of OM is generally accepted.
It occurs due to cellular and humoral sensitization to “beyond-barrier” antigens of uveoretinal tissue (retinal S-antigen or PEP-65 pigment epithelium antigen). Violation of the blood-ophthalmological barrier during penetrating trauma leads to the entry of antigens into the lymphatic and bloodstream; depending on the dose, sensitization of both the other eye and the body as a whole can occur. An autoimmune pathological process occurs.
This is also facilitated by genetic predisposition, connection with histocompatibility antigens with a predominance of HLA-A11 antigens, erythrocyte antigens of the ABO system - blood group I (0), as well as a disorder of the body’s immune system, characterized by an imbalance of T-lymphocyte subpopulations.
Trauma and surgery
Not any injury can lead to sympathetic ophthalmia, but more often that which affects the limbus area, to which the internal membranes are adjacent, prolapse and are often pinched in the scar. In case of injury, it is very important to urgently (no more than within 24 hours) receive qualified microsurgical care. When analyzing cases of the disease, we found that patients sought help late and operations were not always performed at the proper level. This was indicated by rough scars.
OM can also occur after planned surgery, more often during cataract extraction; a risk factor for sympathetic ophthalmia is repeated operations, especially interventions after injuries. Such patients require special medical supervision.
Is an injured eye dangerous or not dangerous for the other eye?
This question arises every time before an ophthalmic surgeon when a penetrating injury occurs, complicated by damage to the inner membranes of the eye, those tissues that have the properties of autoantigens. There are practically no clear clinical signs on the basis of which a doctor can foresee the possibility of developing OM. The long search for laboratory tests to predict OM has so far been unsuccessful. This is not surprising if we take into account the autoimmune genesis of the disease. Doctors are guided by a combination of clinical risk factors, taking into account the nature of the injury, the adequacy of the initial surgical treatment and subsequent drug treatment.
Time before and time after
However, the occurrence of the disease may not be limited to a 2-week “incubation period”. This is facilitated by favorable conditions that create violations of the blood-ophthalmological barrier, its late restoration, repeated damage to the uveoretinal membranes containing autoantigens, their migration along the lymphatic pathways of the conjunctiva and the formation of an immunopathological reaction in the eye. Therefore, OM can occur several months, or even years after an episode of penetrating trauma. Therefore, the patient should know that even a small blunt injury (a blow with a fist, a ball) can result in a new surge of autoimmunization, a disease of the second, fellow eye. I recently had a 70-year-old patient whose eye became inflamed after 50 years. Unfortunately, after a penetrating complicated injury to one eye, the threat of OM remains for life.
The rarity of CO, as well as its late occurrence, lead to the fact that only 25 percent. cases, the diagnosis is made in the first week after the appearance of initial signs of the disease. Hence 10-15 percent. unfavorable outcomes of SO.
Thoughtful treatment
The course of OM can be acute, that is, relapse-free, or chronic—sluggish or recurrent. The former is more often observed with the milder, serous form of sympathetic iridocyclitis. With uveoneuroretinitis, serous-plastic iridocyclitis, panuveitis, fibroplastic uveitis, a chronic course is often observed. Relapses usually occur in the form of anterior uveitis or chorioretinitis, when focal chorioretinitis becomes diffuse, leading to a sharp decrease in visual function, up to complete loss of vision.
From the first days of the onset of sympathetic ophthalmia, it is necessary first of all to assess the condition of the injured eye and decide on the need for its enucleation. If the sympathetic eye turns out to be blind and unpromising for vision, it should be removed immediately. However, enucleation is not recommended and is not performed if the eye has proper light projection or residual visual acuity and there is no retinal detachment.
Immediately when the first signs of inflammation appear in the fellow eye, the patient is prescribed corticosteroids locally and orally (dexamethasone, prednisolone). In severe cases, cytostatics (cyclosporine) are added, in recurrent cases - hemosorption, plasmapheresis. The dosage of corticosteroids is determined by the age, body weight of the patient, and the severity of the disease. Inadequately low doses can lead to a chronic course and relapses. Violation of the steroid use regimen or sudden cessation of treatment leads to severe relapses with a sharp decrease in vision. Drug treatment is carried out for a long time, at least 6 months (on average 8-9 months), sometimes up to 1-2 years, depending on the course of the process.
Prevention of sympathetic inflammation
For this, the following is extremely important:
timely, qualified primary surgical treatment of penetrating eye injuries, early (from the first days) active treatment with corticosteroids that suppress local and systemic autoimmune reactions, timely enucleation of the blinded injured eye in the absence of effect from drug treatment.
* * *
The experience available at the Moscow Research Institute of Eye Diseases named after. Helmholtz, allows us to obtain a fairly high percentage of cured patients with sympathetic ophthalmia. However, with proper alertness, physician literacy, timely treatment and patient referrals, these numbers can be even higher.
Prepared by Albert Khisamov, corr. "MG". Photo by Alexander Khudasov.
Treatment and prognosis
Therapy boils down to the use of drugs to dilate the pupil of the eye (for example, atropine sulfate), as well as glucocorticosteroids. If treatment is started at the initial stage of the disease, then inflammation is effectively reduced, and in some cases the pathology recedes.
Glucocorticosteroids are prescribed in the form of retrobulbar injections or installations), as well as intramuscularly. In severe cases, cytostatics are required to suppress the process.
In case of bacterial infection of the eye, a course of antibacterial agents is recommended.
Additionally, the treatment program includes absorbable drugs and other means and methods. The prognosis is serious: blindness among patients reaches 40-80%.
Sympathetic ophthalmia
Sympathetic ophthalmia Penetrating wounds in the area of the cornea and sclera or in the area of the ciliary body, complicated by post-traumatic uveitis Previous intraocular operations - cataract extraction, iridencleisis, operations for retinal detachment, vitrectomy, etc. Perforation of a purulent corneal ulcer Eye injury complicated by endophthalmitis Disintegration of melanoma of the choroid (very rarely).
Sympathetic serous iridocyclitis - mixed injection of the eyeball, whitish or pigmented pre- Sympathetic fibrinous-plastic iridocyclitis - pronounced mixed injection of the eyeball, rapid formation of anterior and posterior synechiae, which leads to fusion and fusion of the pupil, bombardment of the iris, secondary glaucoma, sometimes hypotension develops and subatrophy of the eyeball. Mixed form: in the fundus there are small yellowish-white drusen-like foci, signs of exudative choroiditis in the form of large yellowish-white foci covered by an edematous retina.
Biomicroscopy (turbidity of the corneal endothelium, isolated precipitates, sluggish pupillary reaction, pigment granules on the anterior capsule of the lens) Ophthalmoscopy (papillitis, neuroretinitis with hyperemia and edema of the optic nerve head). Differential diagnosis. Sympathetic irritation associated with an oculo-ocular reaction (lacrimation, photophobia, conjunctival or perilimbal injection of ocular vessels, no signs of inflammation).
Local instillation of atropine (1% solution 3-4 times / day), glucocorticoids (0.1% solution of r-dex-samethasone 5-6 times / day) Subconjunctival and parabulbar injections of dexamethasone 0.5 ml every day ( course of treatment - 8-12 injections) Electrophoresis with prednisolone using the endonasal technique (15-20 sessions) Glucocorticoids, for example prednisolone initially 25-30 mg/day with a further dose reduction by 2.5 mg after 5 days to 15 mg /day, then - by 1.25 mg after 5 days. The total dose per course of treatment for adults is 700-1,000 mg, for children - 500-700 mg. Treatment with glucocorticoids is carried out against the background of an antidiabetic diet, the administration of potassium salts, calcium, vitamin C, under the control of blood sugar levels. The duration of local treatment of fresh forms is 6-12 months, general treatment - 2-6 months. If there is resistance to treatment with glucocorticoids - cytostatics (cyclophosphamide 100-125 mg / day for 1-2 months under hemogram control). Surgical treatment is enucleation in the absence of vision.
The disease occurs at any time after a penetrating wound (from 2 weeks to tens of years), more often - after 1-2 months. The course is chronic, recurrent. The frequency of exacerbations varies from 1-2 in 5-10 years to 1-2 annually. In case of untimely treatment, the disease leads to loss of the eye. The prognosis is more favorable for neuroretinitis and serous uveitis. Prevention Timely enucleation of the blind injured eye (especially against the background of recurrent chronic uveitis) Application of modern microsurgical low-traumatic methods of primary surgical treatment of the injured eye in combination with the prescription of adequate anti-inflammatory therapy in the postoperative period to prevent the development of severe uveitis.
Sympathetic inflammation of the eyes
Etiology of sympathetic inflammation of the eye
. Perforated eye injury, complicated by sluggish chronic iridocyclitis, less often surgical intervention or perforated corneal ulcer. The second, healthy eye becomes ill.
The pathogenesis of sympathetic inflammation of the eye is not entirely clear. It is assumed that there is a uveotropic virus that enters the eye from the conjunctival sac at the time of a penetrating wound and then enters the second eye. In this case, importance is attached to sensitization of the second eye and disruption of nervous trophism. In recent years, the role of toxoplasmosis in the origin of sympathetic ophthalmia has been pointed out.
Symptoms of sympathetic inflammation of the eye. It develops no earlier than 12-14 days, most often 4-8 weeks after injury to the first eye. The disease can occur in the form of uveitis or neuroretinitis. More often, plastic uveitis is observed with signs of irritation of the eyeball, hyperemia of the iris, constriction of the pupil, exudate in the area of the pupil and anterior chamber, posterior synechiae, precipitates, and vitreous opacities. Intraocular pressure is usually reduced, but secondary glaucoma may develop in the future. With sympathetic neuroretinitis, inflammation is more pronounced in the posterior segment of the eyeball.
The course of sympathetic inflammation of the eye. Characterized by slow progression with periods of subsidence and exacerbation of the process. Changes in the refractive media and the retina contribute to a decline in visual function.
Recognition of sympathetic inflammation of the eye
It is not difficult if the process develops in the second eye after a penetrating wound to the first eye. The diagnosis is confirmed by histological examination of the damaged eye.
Prevention of sympathetic inflammation of the eye. Timely enucleation of the injured eye (no later than the 14th day after injury). Indications: severe eye injury, blindness, symptoms of sluggish iridocyclitis, hypotension, lack of positive dynamics of the process. Preventive measures also include timely and thorough treatment of penetrating wounds and their treatment.
Treatment of sympathetic inflammation of the eye . Local mydriatic agents in the form of drops, ointments, powder for hypotension, miotic agents for hypertension. Cortisone in a 0.5% solution once a day in the form of drops, subconjunctival injections of 0.2 ml 1-2 times a week. In the regression stage, instillation of a 3% solution of potassium iodide 3 times a day, dionin 2-3 times a day in a 1-6-10% solution. Leeches on the temple. General treatment is antibiotics intramuscularly and orally (penicillin 150,000-200,000 units 2-4 times a day, for a course of 6,000,000-7,000,000 units; streptomycin 250,000-500,000 units 1-2 times a day, for course 5,000,000-8,000,000 units, tetracycline 100,000-200,000 units with nystatin 0.1 g 4 times a day for 5-10 days orally, chloramphenicol up to 4 g per day for adults, monomycin, erythromycin) . Prednisolone according to the scheme: 5 days, take 1 tablet 4 times a day, 5 days, 1 tablet 3 times a day, 5 days, 1 tablet 2 times, then 5 days, 1 tablet 1 time a day. While taking prednisolone, a salt-free diet with an increase in the amount of protein is recommended, and potassium acetate in solution is taken orally. For 3-4 days before stopping prednisolone, as well as 3-4 days after stopping the drug, ACTH is sometimes prescribed intramuscularly at 10-60 units 2 times a day, for a course of 300-1200 units. Sulfonamide drugs, butadione in the acute period, osmotherapy, and rubbing in gray mercury ointment are indicated.
The prognosis of sympathetic inflammation of the eye depends on the timeliness of treatment. Currently, the use of antibiotics, sulfa drugs, and corticosteroids has significantly improved the prognosis. The prognosis for neuroretinitis and serous uveitis should be considered more favorable.
Types of ophthalmoscopy
There are different methods of ophthalmoscopy. The selection of a specific technique is carried out on an individual basis. Either one method of ophthalmoscopy or a combination of the following methods can be used.
Straight
A technique in which the eye is examined under high magnification. Magnification is achieved by using a special slit lamp attachment (examination equipment). Initially, the doctor checks the bundle of fibers that are diverging.
After this, the doctor examines the disc. He then examines the entire retina, starting from the middle. The main advantage of this technique is a strong increase in the bottom. Thanks to this, the doctor can detect even minor deviations from the normal state.
The disadvantages of the procedure include the fact that it does not provide accurate information about the presence of inflammatory processes in the retina. Also, the examination is aimed, for the most part, at studying the middle of the retina, which negatively affects the completeness of information about certain diseases (retinal detachment may not be detected).
Direct ophthalmoscopy is the most common way to study the fundus of the eye. It is used in most situations, but other techniques are usually used along with it.
Reverse
To perform such an examination, devices with special built-in lenses are used. Such optics are equipped with cameras that transmit images to a monitor. The examination is performed at a short distance from the patient's eye. The ophthalmologist sees a vertically reflected image. For this reason, this technique is called reverse ophthalmoscopy.
A similar examination method is used in situations where a person requires surgery on the retina or eyeball. The advantages of the procedure are that a clear picture is displayed on the monitor. In addition, reverse ophthalmoscopy allows you to effectively examine the entire area of the retina (including the most distant areas). This examination can be carried out even if the lens is cloudy.
The main disadvantage of the technique is weak magnification. The image is magnified only 5 times, while direct ophthalmoscopy provides 15 times magnification.
Biomicroscopy
The examination is performed using a slit lamp. The device dramatically changes the contrast between illuminated and unlit areas. The procedure makes it possible to determine the condition of the patient’s eyes (examine the corneal tissue, retina, lens, nerve). Biomicroscopy is aimed at identifying the presence of foreign bodies in the organs of vision after injury. It is often performed for patients who have gotten glass, sand, or metal particles into their eyes.
Laser
A modern method of ophthalmoscopy, which has recently become increasingly widespread. A laser beam is delivered to the patient's vision. The generated image is transmitted to a computer monitor. This technique makes it possible to detect pathologies at the initial stages. Laser ophthalmoscopy can be performed even with a cloudy lens, which is considered a significant advantage of this method. The entire examination can be recorded on camera.
This technique provides the greatest accuracy of results. However, the price of such an examination is quite high. The high cost is due to the use of a laser, as well as the general complexity of the examination.
Symptoms of sympathetic ophthalmia
The very first symptoms usually begin to appear very slowly. The disease may not make itself felt for several days or even weeks. At the initial stage of development of the pathology, the symptoms are quite unclear and vague. Initial signs include:
- slight pain;
- photophobia;
- mild decrease in visual function.
Symptoms are most often observed in the sympathetic eye. In this case, in the affected organ there is a decrease in vision and slight chronic discomfort. These phenomena increase the need for examination and constant monitoring of the uninjured eye, especially if there is prolonged inflammation and pain after surgery.
In addition to signs of irritation of the visual organ (pain, eyelid spasm, lacrimation, photosensitivity), the following occurs:
- eyeball injection;
- swelling of the iris;
- constriction of the pupil;
- formation of posterior adhesions;
- vitreous fogging;
- accumulation of fluid in the anterior membrane of the eye.
After this, a planar connection of the iris with the upper region of the lens begins, complete or partial closure of the pupil, and the formation of anterior synechiae that close the angle between the iris and cornea.
Over time, the pressure in the eye cavity increases and glaucoma begins to develop. In some cases, there is a strong decrease in intraocular pressure, which, in turn, can lead to subatrophy of the eye.
If iridocyclitis has a serous form, then the signs of sympathetic ophthalmia are weakly expressed. In this case, small precipitates with a gray tint appear in the area of the posterior wall of the cornea, while adhesions are observed very rarely. This type of disease has a more favorable prognosis, but it is much less common.
Iridocyclitis usually develops very slowly. Often, constant exacerbations of the disease are replaced by long-term remissions. Most often, the disease continues for several years. An acute and rapid course of the disease is observed quite rarely.
Types of illness
The following types of sympathetic ophthalmia are distinguished:
- Serous - this form occurs with development. It occurs less frequently than with plastic iridocyclitis and has a milder course. Most often, proper therapy leads to slowing down and stopping the process, as well as preserving the basic functions of the eye.
- Neuritic is the rarest form, which is an independent disease. This pathology is characterized by an asymptomatic onset and absence of changes in the anterior part of the organ of vision. Symptoms of papillitis and mild neuritis are observed in the fundus. The peripapillary part of the retina and the optic nerve head are hyperemic, tissue dullness develops, and the clarity of the contours is impaired. Arteries and veins begin to dilate. Color sensitivity decreases sharply, and the blind spot area increases. Severe photophobia is observed. With timely treatment, the disease progresses quite favorably, and in most cases vision can be preserved.
- Mixed is the most common form of this pathology. In addition to severe plastic iridocyclitis, serous exudation or. Mixed forms of the disease rarely result in complete recovery. Most often, the prognosis of the disease is unfavorable - complete blindness develops.
Symptoms of sympathetic ophthalmia
The very first symptoms usually begin to appear very slowly. The disease may not make itself felt for several days or even weeks. At the initial stage of development of the pathology, the symptoms are quite unclear and vague. Initial signs include:
- slight pain;
- photophobia;
- mild decrease in visual function.
Symptoms are most often observed in the sympathetic eye. In this case, in the affected organ there is a decrease in vision and slight chronic discomfort. These phenomena increase the need for examination and constant monitoring of the uninjured eye, especially if there is prolonged inflammation and pain after surgery.
In addition to signs of irritation of the visual organ (pain, eyelid spasm, lacrimation, photosensitivity), the following occurs:
- eyeball injection;
- swelling of the iris;
- formation of posterior adhesions;
- vitreous fogging;
- accumulation of fluid in the anterior membrane of the eye.
After this, a planar connection of the iris with the upper region of the lens begins, complete or partial closure of the pupil, and the formation of anterior synechiae that close the angle between the iris and cornea.
Over time, the pressure in the eye cavity increases and glaucoma begins to develop. In some cases, there is a strong decrease in intraocular pressure, which, in turn, can lead to.
If iridocyclitis has a serous form, then the signs of sympathetic ophthalmia are weakly expressed. In this case, small precipitates with a gray tint appear in the area of the posterior wall of the cornea, while adhesions are observed very rarely. This type of disease has a more favorable prognosis, but it is much less common.
Iridocyclitis usually develops very slowly. Often, constant exacerbations of the disease are replaced by long-term remissions. Most often, the disease continues for several years. An acute and rapid course of the disease is observed quite rarely.
Types and classifications
Sympathetic ophthalmia has the following forms of development:
- Serous. Characterized by the occurrence of serous iridocyclitis. Most often, therapy in this case gives a good prognosis and the progression of the disease stops. Occurs with average frequency.
- Neuritic. It is diagnosed quite rarely and is an independent pathology. The onset of progression is often imperceptible and asymptomatic; after some time, mild neuritis appears. Dullness and swelling of the tissues and redness occur. It is usually cured with complete restoration of visual functions only in half of the cases.
- Mixed. It occurs more frequently than those listed and combines the characteristics of both forms. In most cases of therapy, the prognosis is favorable and most often ends in complete recovery of the patient.
Serous form of sympathetic ophthalmia
How to treat sympathetic ophthalmia?
Remember! Very often, sympathetic ophthalmia can lead to complete removal of the affected eye.
But usually ophthalmologists strive to preserve the organ, regardless of whether it will at least partially perform its functions or whether the patient is in danger of complete blindness.
If vision remains at a sufficiently high level as a result of the disease, removal of the eye (enucleation) can be carried out if the ophthalmologist is confident in the possibility of the development of sympathetic inflammation.
Although in this case it is difficult to predict such a development of events, and sometimes an erroneous diagnosis is made, which leads to the removal of the eye unnecessarily.
Initially, the eye is treated by using immunosuppressive or immunocorrective therapy.
In such cases, immunomodulators are used, which are taken strictly under the supervision of the attending physician. Among these drugs are:
- cytostatics,
- glucocorticosteroids,
- antimetabolites,
- antilymphocyte serum.
These medications can be used either topically or included in a systemic course of treatment.
Need to know! During treatment, uveitis is prevented or eliminated, for this purpose mydriatic drugs are used. This complex of treatment allows maintaining visual acuity in 9 out of 10 patients.
In some cases, surgical intervention is appropriate, during which vision is also restored, and after the operation the patient undergoes an additional course of treatment using anti-inflammatory drugs.
It may be necessary to use antiallergic drugs (if during treatment it turns out that a person has allergic reactions to some drugs). Treatment of sympathetic ophthalmia is carried out only in a hospital setting, while the quality of the services provided depends on the level of the clinic, and the possibility of preserving vision directly depends on this.
For example, in some ophthalmology centers there may be no treatment with immunomodulatory drugs, and specialists immediately begin to insist on removing the eye to prevent the spread of inflammatory processes.
23.3.5. Sympathetic inflammation
Penetrating injuries to the eyeball entail severe complications, the occurrence of which poses the risk of not only the death of the injured eye, but also the development of sympathetic ophthalmia of the second, healthy eye, which is observed in 0.1-0.2% of cases after a penetrating injury and 0. 06—0.07%—after intraocular operations. Sympathetic (sympathetic) ophthalmia is an inflammation of the second, hitherto healthy eye in response to injury to the first. Inflammation most often manifests itself in the form of sluggish fibrinous-plastic iridocyclitis.
The first symptoms of sympathetic inflammation appear no earlier than 14 days later; later symptoms can occur after many months and even years. In a healthy eye, mild pain, photophobia, and mild (noticeable only during the examination) pericorneal vascular injection are initially noted. Later, precipitates appear on the posterior surface of the cornea, the clarity of the iris pattern is disrupted, the pupil narrows, posterior synechiae are formed, and fusion and fusion of the pupil occur. Ocular hypertension is replaced by hypotension, and then subatrophy of the eyeball. The clinical and histological pictures of inflammation of the first and second eyes are very similar. Inflammation in the first, injured eye is called “sympathetic”, and in the second - “sympathetic”. Sympathetic ophthalmia may manifest as neuroretinitis or focal choroiditis and be complicated by retinal detachment. Currently, the leading role in the development of sympathetic ophthalmia of autoimmune reactions with the formation of delayed-type hypersensitivity and the formation of humoral antibodies to uvearetinal antigens with the subsequent development of secondary immunological failure has been established.
Due to the use of a wide arsenal of powerful anti-inflammatory and steroid drugs, timely surgical operations (skilled treatment of wounds, removal of cataracts, foreign bodies, etc.) at a high technical level, the clinical manifestations of sympathetic ophthalmia, the nature of its course and the incidence of complications have undergone changes and significantly differ from those in cases previously described in the ophthalmic literature.
Removal of the blind injured eye, which is a source of autosensitization, can serve as a reliable measure to prevent the development of sympathetic ophthalmia in the healthy eye if the operation was performed within 14 days after the injury.
The decision to remove the eye is made if, 2 weeks after the injury, the low-grade fibrinous-plastic inflammation does not subside. It is difficult to decide to take such a step when the damaged eye is sighted. If signs of sympathetic ophthalmia occur in a healthy eye, the injured eye is removed only if it is blind. In the presence of even very poor vision, enucleation of the injured eye is not performed. The prognosis of sympathetic ophthalmia is always very difficult, and it may happen that subsequently this eye will be the best.
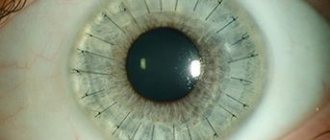
Diagnosis of sympathetic ophthalmia is often difficult, especially with the development of inflammation in the fellow eye in the late stages after injury, as well as with erased forms and localization of the process in the posterior parts of the eyeball. Risk factors for the development of this pathology are localization of wounds in the corneoscleral zone, iris loss, lens trauma, retinal detachment, and the development of post-traumatic iridocyclitis. It has been established that most often sympathetic ophthalmia develops in the 1st-2nd months after injury (57.6% of cases) and 92.5% of all cases occur in the first year.
When the first signs of inflammation appear in the fellow eye, conservative therapy begins with the administration of steroids locally and orally. Locally - dexamethasone in the form of instillations, under the conjunctiva and parabulbar. It is possible to use phono- or electrophoresis of a 1% solution of prednisolone endonasally. The use of mydriatics is mandatory.
The duration of therapy with steroids taken orally is determined by the clinical manifestations of the inflammatory process. Thus, for various forms of iridocyclitis, the initial dose of prednisolone in adults is on average 40-80 mg (8-12 tablets) per day, in children - 25-40 mg with a gradual reduction every 5 days by 5 mg to 1/4 tablet. In order to prevent relapses, non-steroidal anti-inflammatory drugs (indomethacin, ibuprofen, etc., 50-75 mg per day) are used during treatment with steroids, as well as for 2-3 months after the end of the course of steroid treatment. The duration of the course of treatment (prednisolone, metipred, etc.) is on average 75-80 days. Thus, the duration of local treatment is at least 12 months, and general - 6 months. Premature cessation of treatment leads to early relapses and a chronic course. If inflammation affects the entire vascular tract of the anterior and posterior segments of the eye, then steroids are taken for a long time, for 1-2 years, in a maintenance dose of 10-15 mg (for prednisolone). The choice of drug is determined by the clinical form of sympathetic ophthalmia and the level of corticosteroids in the patient’s blood plasma. For iridocyclitis, it is preferable to use prednisolone, for uveaneuroretinitis - polcortolone, kenacort, for panuveitis - metipred. In some cases, it is necessary to prescribe cytostatics (cyclophosphamide 50 mg 2 times a day for 1-2 months). Decaris, sodium nucleinate, pyrogenal, liquid aloe extract for injection, FiBS, fractional blood transfusion, etc. are used as immunostimulants.
All patients with sympathetic ophthalmia require constant follow-up by an ophthalmologist throughout their lives. If there is a need for cataract extraction, surgery to form the pupil or other interventions, they can be performed only during the period of remission (at least 6-12 months after an exacerbation) against the background of conservative therapy and under strict immunological control.
- < Back
- Forward >
Interchangeability of the VAZ 2108 and VAZ 2106 generator
The idea of replacing a generator on a classic is as old as the history of the car itself, because everyone who installs more bells and whistles on their own car than a weak Chinese radio, the native 42A G-221 is no longer enough for everyone.
True, even those who neglect the hassle of installing a more powerful generator are annoyed by the weak low beam at idle and poor battery charge. Once, an acquaintance fitted me with a 55A generator on a ball and the idea arose about telling you how to install it in our classic.
Having scoured the Internet to find at least something about installing and connecting it to a car, I didn’t find anything useful, a lot of comments like “Plug it in and forget it” or long discussions of professional electricians, but they spoke in a language that would suit a simple Russian to a person, it’s like a Chinese song, nothing is clear.
In this regard, it was decided to write an understandable article for ordinary people in order to help them do this simple procedure of replacing the generator themselves, without any problems and special skills in working with electricity, but with their hands. It is important to know: There are many alternatives to a standard generator, since with the appropriate skills, means and desire it is possible to install any generator. In the provided article I examine only “economical” VAZ generators from other models, because:
- They are cheaper.
- They are more common.
- They are easier to change - you don’t need to find or make any special fasteners and completely change the electrical system.
Prevention
It is quite difficult to prevent the occurrence of sympathetic ophthalmia. This is due to its unpredictability and difficulty of forecasting. The disease occurs infrequently and is not always a consequence of injury. Therefore, the main preventive measures include the following:
- Eliminate eye diseases in a timely manner;
- Avoid situations involving a high risk of eye injury;
- Properly carry out all necessary hygiene procedures and avoid infectious contamination;
- Monitor the condition of your visual system and undergo preventive examinations with an ophthalmologist at least once a year.
Sympathetic ophthalmia: symptoms, diagnosis, treatment
Sympathetic ophthalmia is a non-purulent inflammation that develops in a healthy organ of vision due to injury to the second eye or ophthalmic surgery performed on it.
The process develops and manifests itself very slowly; in some cases, the appearance of severe symptoms is preceded by a period of several weeks to several months. The danger of the pathology is that it can lead to the loss of the inflamed eye, while the main treatment is aimed at healing the diseased paired organ.
Reasons for the development of pathology
The mechanism and causes of the development of the inflammatory process are not precisely known. There are several equal theories in this area:
- The pathogen infects a healthy eye through the blood, that is, it is uveotropic.
- The pathology is a consequence of a weakening of the body's protective functions, immune disorders or an autoimmune allergic reaction.
- Inflammation is associated with dysfunction of the nervous trophism.
At the same time, researchers identify a number of main factors that can lead to the development of the disease:
- penetrating and blunt eye injuries;
- penetrating wounds and ulcers of the cornea;
- ophthalmological operations;
- contusions;
- subconjunctival rupture of the sclera;
- malignant tumors.
Reduced intraocular pressure increases the risk of developing sympathetic ophthalmia, increased and normal - reduce it.
A phenomenon that requires immediate treatment, or why the eyes fester.
Reduced intraocular pressure more often leads to the development of the disease
Carefully! A dangerous disease that can significantly affect the quality of vision is retinoschisis of the retina.
Prevention and prognosis
Considering the penetrating nature of eye injuries, in which sympathetic ophthalmia develops, such a diagnosis is rare in ophthalmological practice. However, according to statistics, up to 80% of cases of diagnosing a disease, it ends unfavorably for the patient, i.e. complete blindness.
At the same time, the probable causes of the spread of inflammation also include other factors not related to injuries, so it is almost impossible to prevent the pathology. Experts in this field advise adhering to basic preventive measures aimed at preventing the disease:
- compliance with personal safety rules to avoid eye injuries;
- systematic examination by an ophthalmologist;
- compliance with all recommendations for the treatment of diseases of the organs of vision, incl. infectious and other nature;
- seek medical help if any problems with the visual system are identified;
- compliance with eye hygiene rules;
- refusal of self-medication.
Antibacterial drug of the fluoroquinolone group - instructions for use of Signicef eye drops.
Diagnosis of pathology takes into account the patient’s complaints, and includes a visual examination and medical examination of the cornea, lens and tissues around the site of inflammation.
When white light is not nice or establish the true causes of photophobia of the eyes.
The symptoms and treatment of retinal detachment are described in detail in the article.
Sympathetic ophthalmia is one of the most dangerous, unpredictable and little-studied pathologies of the visual organs. The mechanism of spread of the inflammatory process from a damaged and/or blind eye to a healthy eye has not yet been precisely established, but the risk of developing this process increases with penetrating wounds of the paired organ.
The article is for informational purposes only and cannot be considered for independent diagnosis and treatment. Before carrying out any treatment procedures, it is necessary to consult with specialists in the field of ophthalmology.
Causes of the disease
Typically, sympathetic ophthalmia occurs in conjunction with iridocyclitis, which can be provoked by:
- trauma to the visual organ of various etiologies;
- corneal ulcer;
- subconjunctival rupture of the sclera;
- intraorbital benign;
- malignant neoplasms;
- less often, iatrogenicity is the cause.
An autoimmune disorder of the eye structure plays a significant role in the occurrence of pathology. In this case, antibodies are produced to the S-antigens of the retina, pigment epithelium and uveal tract.
Scientists have proven that the process of occurrence of sympathetic ophthalmia is directly dependent on HLA class II antigens. The immunomorphological causes of inflammation are delayed-onset hypersensitivity with the presence of type 1 Th lymphocytes.
Endogenous internal toxins, which arise as a result of apoptosis of uveal tract tissue, are identified as etiological factors in the development of this disease. This phenomenon provokes the involvement of a healthy eye in the inflammatory process.
In addition, various enzymes, such as trypsin or zymase, can be causative agents of the disease. Another reason is infection of the structure of the eyeball with the herpes virus. This can cause the development of sympathetic ophthalmia, which will subsequently give way to endophthalmitis.
Treatment
In cases of negative effects of light rays on the cornea, action should be taken immediately. First of all, the patient must be provided with peace, placed in a darkened room and limited from eye strain.
To relieve pain, use an eye ointment or gel with an anesthetic effect. Compresses on the eyes using Erythromycin or Tetracycline are also effective.
It must be remembered that the ointment can inhibit the restoration of mucous membranes.
After eliminating the pain, drops with antibacterial properties should be used to help relieve inflammation. Such drugs are prescribed only by an ophthalmologist. You can also use drops like artificial tears, since additional hydration of the mucous membrane will not be superfluous. During the restoration of the corneal membrane, you should completely refrain from performing any types of work or stress on the visual organs.
It is important to remember that with electroophthalmia it is prohibited:
- rubbing your eyes, as such actions only complicate the problem and cause even more irritation;
- rinse your eyes with running water, this can lead to infection in the eye membranes;
- independently use traditional medicine methods for basic treatment;
Treatment of the disease
After visual contact with an ultraviolet source, the patient needs first aid. If there is no first aid kit nearby, then it is enough to apply a lotion to your eyelids with cold water or tea leaves. This will reduce the severity of the burn. However, instillations should not be done without consulting a doctor, because self-medication can only worsen the patient’s condition.
Further treatment of electroophthalmia involves the use of the following groups of drugs:
- local anesthetics (Dicaine, Alcaine, Tetracaine, Lidocaine) to relieve severe pain;
- antibacterial eye ointments (Tetracycline, Gentamicin) or drops (Tobrex, Tobradex, Levofloxacin) to prevent secondary infection;
- non-steroidal anti-inflammatory drugs (Diclofenac, Indocollir, Prenacid, Meloxicam) to eliminate corneal clouding, reduce the severity of pain and symptoms of inflammation (redness, swelling, itching). The drugs are prescribed orally;
- vasoconstrictor drops (Vizin, Proculin, Visoptin). The drugs help reduce swelling of the cornea and eliminate redness of the eyes;
- the drugs Solcoseryl and Actovegin promote rapid healing of the cornea.
Important! You should not self-medicate with electroophthalmia. After all, incorrectly selected medications can provoke a bacterial infection and decreased vision.
Causes
Provided that traumatic iridocyclitis is observed in one eye or the eye has been subjected to perforated injuries and wounds, corresponding disorders occur on the paired organ.
Contusions and the appearance of tumors can also serve as a prerequisite for the development of the disease. The second case is considered extremely rare.
Carefully! Sympathetic ophthalmia can also appear on a healthy organ if severe anterior uveitis is diagnosed in the affected eye. This often leads to the development of the same disease on the paired organ, even if no physiological prerequisites for the occurrence of the disease have been established
This often leads to the development of the same disease on the paired organ, even if no physiological prerequisites for the occurrence of the disease have been established.
Main symptoms of the disease
If you begin to develop ophthalmitis, in this case, the symptoms of this pathology can be expressed as follows:
- floating spots on the eye;
- decreased visual acuity;
- pain in both eyes;
- increased sensitivity to light.
- redness;
- headache;
- retinal detachment in severe cases.
A clear record of past penetrating trauma or surgery in one eye with subsequent inflammation raises suspicion. Therefore, we recommend conducting an emergency examination at Ophthalmology 1ST, where experienced specialists will be able to identify the onset of development of eye inflammation, the symptoms of which can only be detected with special equipment.
These may include signs such as a strong reaction in the anterior chamber (front) of both eyes with large fatty deposits appearing on the cornea (fatty deposits), white-yellow lesions called Dahlen-Fuchs nodes in the choroid, thickening of the uveal tract (middle layer eyes). Sympathetic ophthalmia may be accompanied by swelling of the optic disc (papilloedema), cataracts, glaucoma, non-pigmented white patches on the skin, and patches of white eyelashes (poliosis).
Treatment methods
Ophthalmia is an autoimmune disease, so conservative treatment is aimed at suppressing the immune system. For this purpose, glucocorticosteroids, cytostatics, antimetabolites and sulfonamides are used. These drugs are used under the control of the immune system because they have a wide range of side effects. Drug therapy is not able to completely cure the patient, but can prolong the period of remission and preserve vision.
Surgical treatment methods are based on the removal of the affected organ in order to save the other eye and remove the source of the autoimmune effect. In this case, vision can be saved. In preparation for such an intervention, drugs that suppress the immune system, anti-inflammatory and anti-allergic are also used. This method must be used after a thorough examination of the patient and confirmation of the diagnosis.
Sympathetic ophthalmia (SO) is a lesion of the choroid (uveal tract) of the healthy eye following penetrating damage to the other eye. As a consequence of eye injuries, OM develops relatively infrequently, in approximately every fiftieth case, but in most cases it results in loss of vision.
The cause of damage to a healthy eye in OM is the close neuro-reflex connections between these paired organs. This state of affairs implies that if one eye is susceptible to any disease, then in due time pathological changes will affect the other, until then healthy eye. OM is considered as a manifestation of autoallergy, which is confirmed by the presence in the blood of patients of circulating antibodies to the elements of the choroid. Certain importance is attached to disorders of nervous trophism.
Risk factors for OM are:
- penetrating injuries of the cornea, sclera, ciliary body, complicated by uveitis;
- intraocular surgical interventions;
- perforation of a purulent corneal ulcer;
- eye injuries complicated by endophthalmitis.
OM usually begins no earlier than two weeks after the injury and is characterized by a steadily progressive course, with periods of exacerbations followed by remission. Sometimes the disease can last for years. Blindness occurs in approximately sixty patients out of a hundred. Prevention of OM involves enucleation of the injured eyeball.
Symptoms of OM are often indistinguishable from the symptoms of other ophthalmological diseases, but the main difference is that a healthy eye becomes ill against the background of another, already diseased eye. It should be remembered that in every third case CO occurs in an erased form. Symptoms of disease activity:
- blepharospasm (involuntary squinting of the eyes, difficult to overcome by volitional effort);
- constriction of the pupil;
- severe lacrimation;
- decreased visual acuity;
- photophobia;
- the appearance of spots on the cornea of the eye;
- scleral injection.
It is unusual to have all the symptoms at once; usually there are no more than two. The erased form is not clinically manifested and is detected only by biomicroscopy.