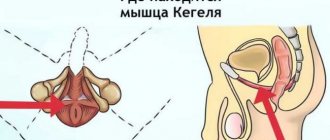
The pubococcygeus muscle (m. pubococcygeus) plays such an important role in the human body that Chinese doctors called it “the gate of life and death.” It prevents pelvic organ prolapse and is responsible for the quality of sexual life in men and women.
The pubococcygeus muscle is one of the pelvic floor muscles.
For hundreds of years, at the court of the Chinese emperor, there were schools where future geishas were taught special techniques to give true pleasure to a man during intimacy. We are talking about training the pubococcygeus muscle, which helps maintain a woman’s intimate health throughout her life.
Where is the pubococcygeus muscle located?
This is one of the muscles of the pelvic diaphragm, which, together with the iliococcygeus, forms the levator ani muscle (m. levator ani). It is a muscle extending from the pubic bone in front to the coccyx in back, m. pubococcygeus is sling-shaped and forms the pelvic floor, surrounding and supporting the bladder neck, anterior rectum, male prostate gland and female vagina. It is located under the skin at a depth of approximately 2.5 cm and is regulated by the pudendal nerve, which, in addition, innervates the pelvic organs and the skin of the perineum. This muscle is very well felt when we cannot go to the toilet for a long time and we have to hold back urination. The pubococcygeus muscle is responsible for contracting the pelvic floor and anus during intimacy. If this muscle is not exercised for a long time, then over time it weakens, causing prolapse and weakening of the adjacent internal organs.
Features of blood supply and innervation
The blood supply to the pelvic floor muscles, including the pubococcygeus muscle, is regulated by the internal pudendal artery a. Pudenda interna. At the lower edge of the urogenital diaphragm, this artery divides into the dorsal and deep artery of the penis (clitoris).
The pubococcygeus muscle is innervated by the muscular branches of the sacral plexus and the pudendal nerve n. Pudendus.
Pelvic floor muscles: myths and controversial issues
Much has been written about pelvic floor training. This topic is of interest not only to yogis (in the context of mastering mula bandha and ashwini mudra) and urologists (in the context of preventing stress urinary incontinence and pelvic organ prolapse), but also to people who are far from medicine and hatha yoga - women who want to recover faster after childbirth or prepare for it.
Apparently, it is precisely because of such popularity of the topic that there are those who want to play on this - to create a new “revolutionary” theory, to act as an innovator, while refuting time-tested methods. It’s good when new ideas have a reliable evidence base, and bad when, under the guise of “expert opinions,” they mislead people who are not knowledgeable about medical issues.
So, a translated interview (original - https://mamasweat.blogspot.ru/2010/05/pelvic-floor-party-kegels-are-not.html) with Katy Bowmen, representing himself as a specialist in the biomechanics of the human body (https://www.alignedandwell.com/katysays/about-2/). The essence of her “innovative” theory is as follows: the failure of the pelvic floor is primarily caused by its sagging due to the fact that the sacrum moves forward, into the pelvis. Since the pelvic floor muscles are attached to the tailbone and to the pubic bone, due to the convergence of these bones, the pelvic floor sags (becomes like a hammock). Kegel exercises strengthen the pelvic floor muscles, while pulling the sacrum inward, causing it to become even more compressed and weakened. The author recommends that instead of Kegel exercises, train the gluteal muscles, which, in her opinion, will pull the sacrum back and stretch the pelvic floor, preventing it from sagging, and also level the position of the pelvis, stretching the inner and back surfaces of the thighs and calf muscles.
Let's try once again to understand this controversial topic and first say a few words about the anatomy and medical aspect of pelvic floor incompetence, and then remember who and why came up with exercises for training the muscles of this part of the body and try to analyze the available data.
The pelvic floor is a collective concept that includes all the anatomical structures that form the floor of the abdominal cavity. The organs located in the pelvis - the bladder, urethra, uterus, rectum and anus - are directly adjacent to the pelvic floor. The thickness of the pelvic floor is not the same throughout.
The pelvic floor is conventionally divided into 4 main layers. In addition to several layers of muscles, the ligamentous and tendon apparatus is of great importance in stabilizing the position of the pelvic floor, forming topographically several levels of support for the pelvic organs (Fig. 1, 2).
Fig.1
Fig.2
The first layer is represented by the peritoneum, covering the walls of the pelvis and partially the pelvic organs. The second layer is the pelvic fascia - fibromuscular tissue that extends from the side walls of the pelvis and surrounds the pelvic organs, which fixes the pelvic organs and stabilizes their position. The peculiarity of the pelvic fascia is that in its structure, in addition to collagen and elastane, there is a large number of long wavy smooth muscle cells that provide contractile
pelvic floor ability. The cardinal ligaments that fix the uterus to the walls of the pelvis are strengthened by collagen, which is part of the walls of arteries and veins. The next layer is called the “pelvic diaphragm” and is represented by powerful striated muscles, among which are the levator ani and coccygeus muscles. The levator ani muscle (m. levator ani) and the coccygeus muscle, connecting with similar muscles on the opposite side, form the pelvic floor. It consists of the pubococcygeus (m. pubococcigeus) and iliococcygeus (m. ileococcygeus) muscles. The pubococcygeus muscle begins from the posterior surface of the body of the pubic bone and the anterior part of the tendinous arch of the levator ani muscle (arcus tendineus levator ani). The latter is a dense connective tissue structure that extends from the pubis to the ischial crest and passes next to the obturator internus muscle. The pubococcygeus muscle is directed horizontally and forms the urogenital hiatus. A group of small muscles that are part of the pubococcygeus extend from the pubic bone to the urethra, vagina, and rectum. These muscles are distinguished as puborectral (m. pubourethralis), pubovaginal (m. pubovaginalis) and puborectal muscles (m. puborectalis). The urethral part is involved in the formation of the external urethral sphincter, and the vaginal and anal parts form the muscular walls of the vagina and the external sphincter of the anus. Posteriorly, the pubococcygeus muscle attaches to the coccyx. The lateral, thinner part of the levator ani muscle is called the iliococcygeus muscle. It originates from the tendinous arch of the levator ani muscle and the ischial crest. On the anterior surface of the sacrospinous ligament (lig. sacrospinosus) is the sacral muscle. The muscle fibers of the opposite sides merge to form the rectococcygeal ligament. This midline suture between the coccyx and the rectum is the platform on which the pelvic organs lie. In a standing position, this muscle area is in a horizontal plane and holds the rectum and upper 2/3 of the vagina. Weakening of the levator ani muscle leads to sagging of the muscle area. In this case, the urogenital hiatus is deformed, increases in size and leads to prolapse of the pelvic organs. The genitourinary or urogenital diaphragm connects the lower branches of the pubic bones in the form of a bridge with the tendon center of the perineum. Covering the urogenital hiatus, the urogenital diaphragm has a sphincter-like effect on the distal part of the vagina; in addition, being attached to the striated periurethral muscles, it participates in urinary continence. In the center of the pelvic diaphragm is the levator foramen (hiatus), through which the urethra, vagina and rectum exit the pelvic cavity. The lowest layer of the pelvic floor is represented by structures that form the urogenital and anorectal triangles, the conventional border between which runs between the tuberosities of the ischial bones. In the urogenital triangle there is a perineal membrane, represented by the deep transverse perineal muscle. The muscles of the genital organs are located outside - the bulbospongiosus, ischiocavernosus and superficial transverse perineal muscles. The anorectal triangle contains the anal sphincter, which connects posteriorly with the anal-coccygeal ligament and anteriorly merging with the superficial transverse perineal muscle. Externally, the pelvic floor is covered with the skin of the vulva and perineum (Fig. 3, 4).
pic 3
pic 4
Pelvic floor muscle insufficiency (PFMI) and genital prolapse (PG) are current clinical and surgical problems of modern gynecology. PG is observed in up to 38.9% of women, according to domestic and foreign authors, and in the structure of gynecological interventions, surgical correction of PG ranks third after benign genital tumors and endometriosis (Comprehensive diagnosis of pelvic floor muscle failure after vaginal delivery. The topic of the dissertation and abstract on the Higher Attestation Commission 14.00.01, Candidate of Medical Sciences Ziganshin, Aidar Mindiyarovich) .
Normally, the strength and elasticity of the pelvic floor structures are sufficient to support the pelvic organs even with an increase in intra-abdominal pressure within the physiological norm.
Dysfunction of two structurally interconnected tissues - muscle and connective tissue - leads to weakening or NMTD, and then to decompensation, against the background of which prolapse manifests itself [8].
According to some data, the appearance of NMTD is preceded by a weakening of the muscle component; according to others, it is a congenital anomaly of the connective tissue structure or connective tissue dysplasia (CTD), which is more significant than birth trauma [15,20].
Traditionally, the development of genital prolapse was associated with heavy physical labor, heavy lifting, during which there is a sharp increase in intra-abdominal pressure, “pushing” the uterus out. Also a risk factor are excess weight and obesity, while the higher the BMI, the more likely the need for surgical treatment and the ineffectiveness of conservative (non-surgical) measures.
However, the vast majority of scientists still assign an important role to pregnancy and childbirth in the development of prolapse. The risk of prolapse is significantly higher in women who have given birth, and its degree is related to the number of prolapses and complications associated with pregnancy and childbirth, including surgical aids during childbirth, rapid labor, perineal ruptures, delivery of a large fetus, etc.
An undoubtedly significant factor predetermining the formation of pelvic organ prolapse is considered to be a defect in the connective tissue that makes up the ligaments of the supporting apparatus of the pelvic organs. This opinion is supported by the fact that genital prolapse affects both nulliparous women and women who have had one uncomplicated birth, as well as men. Weakening of the pelvic muscles is one of the causes of stress urinary incontinence in the stronger sex.
It is also known that connective tissue diseases such as Marfan syndrome and some diseases of the nervous system are associated with genital prolapse, which develops mainly at a young age. Some authors consider pelvic floor incompetence to be a type of hernia, indicating that the likelihood of developing prolapse is higher in women with hernias of other locations.
So, NMTD and its consequences - genital prolapse and weakening of the muscles of the urethra - have been and remain pressing problems in gynecology and urology. For this reason, an important task is to adequately prevent dysfunction of the pelvic floor and promptly initiate measures to prevent muscle weakness in this area.
In the 50s of the 20th century, the American gynecologist Arnold Kegel, working with patients with urinary incontinence, noticed that women with developed perineal muscles suffered from this disease to a much lesser extent. Further clinical studies and observations allowed him to conclude that it was necessary to train the pelvic floor muscles. Kegel developed the so-called “Kegel exercises” and became the author of the invention of the “Kegel Perineometer,” which can be used to measure vaginal pressure.
Kegel recommended doing three times a day for 20 minutes or doing a total of 300 compressions daily. So, if you multiply 60 minutes by 60 seconds, you get 3600 seconds, and if you divide them by 300 contractions, you get a 12-second cycle. In his works, the doctor schematically defines “time pressure” in the form of sine waves, and notes that at the final stage, healthy contractions become “extended.” Thus, using simple arithmetic, we can conclude that he means 6-second contractions.
Is it possible to “retrain” the pelvic floor in that state when overexertion weakness sets in? The pelvic floor musculature is a type of voluntary striated muscle, that is, it is amenable to conscious training, and all the principles and methodology of training muscle strength and endurance are applicable to it. Muscle strain occurs after high-intensity strength training (with heavy weights, for example), when the body's compensatory capabilities are exceeded, or in the absence of an adequate rest period between workouts.
Here are the recommendations for training the pelvic floor muscles given by official medicine: “To improve general muscle strength and power, sedentary, sick or elderly individuals are recommended to perform 1 to 2 sets of 8 to 12 preset exercise repetitions, with 8 to 10 exercises per session , at a frequency of 2 to 3 times per week.” (Can Urol Assoc J. 2010 December; 4(6): 419–424., PMCID: PMC2997838) That is, to improve overall muscle strength and endurance, weak or elderly people are recommended to perform 1-2 sets of 8-12 given repetitions, 8 -10 exercises per session, with a frequency of 2-3 times a week. As you can see, we are not talking about “high-intensity strength training” here, and the onset of overexertion weakness in this case is unlikely.
To date, the effectiveness of pelvic floor muscle training has been confirmed by a large number of independent scientific studies (PMID: 15791633; PMID: 23076935) and others. Some reviews do not even discuss the rationale for using the training, but are talking about choosing the most effective approach for it (PMCID: PMC2997838 ).
That is, Kathy Bowman's statement: “Misunderstanding of pelvic floor issues is so widespread that I am now completely alone with my opinion. But science supports me and this is reasonable, since kegels are just part of our culture. Nobody bothered to check this knowledge.” in fact shows a lack of understanding of the issue by the author himself, and science also confirms this.
Let's return to the “revolutionary theory”, which strongly recommends developing the strength of the gluteal muscles (Which ones - large? Medium? Small?) instead of performing exercises for the pelvic floor muscles. Let's assume that we were talking about the gluteus maximus muscles, which mainly form the relief below the lower back (which is what the article focuses on). Training these muscles is definitely necessary in the postpartum period. During pregnancy, as a result of a shift in the center of gravity, the physiological curvature of the lumbar spine compensatory increases. With low levels of physical activity during pregnancy and lack of rehabilitation exercises after childbirth, pelvic malposition may become permanent. To prevent this from happening, it is advisable to focus on a range of exercises to train the muscles of the lower back and buttocks, including various types of squats, and not to "prevent the sacrum from moving forward." Deep squats and squatting positions, as well as exercises for the inner and back surfaces of the thighs, are undoubtedly beneficial for the condition of the pelvic floor, but from the point of view that they enhance the proprioceptive sensitivity of this area due to the movement of the hip joints and stretching of the muscles and ligaments around them. This work improves blood flow in the pelvic area, activates metabolic and recovery processes.
The gluteus maximus muscle, when contracted, helps to reduce lumbar lordosis, that is, it reduces the forward tilt of the pelvis. The article literally says the following: “The gluteal muscles pull the sacrum back. If these muscles are not pumped up (“no butt”), then the pelvic floor is more susceptible to failure. The absence of lumbar curve is the most noticeable sign of the beginning weakening of the pelvic floor,” which defies logic, as well as the biomechanics of m. Gluteus maximus.
It is also worth noting that not all pelvic floor muscles that need rehabilitation after childbirth have an attachment point on the tailbone. The vast majority of voluntary muscles that maintain the normal position of the pelvic floor are NOT associated with the tailbone, and therefore, there is no need to strive to “pull them back”, making the pelvic floor resemble a hammock. In general, the analogy with a hammock and a trampoline is not entirely correct. When contracting, the pelvic floor is pulled upward and inward, toward the center of the body. When muscles contract, the attachment points do not move towards each other, and even more so the coccyx is not capable of significant displacement separately from the sacrum. The play of movement of the tailbone separately from the pelvis is small, and the pelvis, together with the sacroiliac joints and the sacrum, forms a single structure. So, with an increase/decrease in the severity of lumbar lordosis, this entire structure increases/decreases its inclination as a whole.
So, let's summarize.
1) Training the pelvic floor muscles is a proven, effective method of preventing pelvic floor incompetence and its consequences - urinary incontinence and organ prolapse. Arnold Kegel exercises, like other similar techniques, can and should be performed before, during and after pregnancy, as well as for other indications and simply if the practitioners have the desire.
2) Performing exercises for the pelvic floor and training the gluteal muscles do not exclude, but on the contrary, complement each other. The same applies to exercises to develop flexibility of the hip joints and improve stretching of the back and inner thighs.
3) Knowledge of the basics of biomechanics and anatomy helps you to be critical of various information appearing on the Internet, and to build your practice, guided by common sense and logic, and not by the opinions of newly-minted authorities.
Main functions of the pubococcygeus muscle
The pubococcygeus muscle plays an important role in the health of the pelvic organs, preventing their prolapse. Its main function is to control the opening and closing of the urethra, anus, prostate gland in men and vagina in women. If it weakens, problems such as urinary incontinence, colon prolapse, and uterine prolapse may occur. The second name is m. pubococcygeus is the “muscle of love”, because it has a great influence on the sex life of both men and women. A strong, trained pubococcygeus muscle enhances the pleasant sensations during intimacy by stimulating blood flow to the genitals.
Muscle functions in women
A strong intimate muscle reduces the likelihood of perineal ruptures during childbirth and helps reduce the time of delivery. It provides control over the anal sphincter and allows you to maintain vaginal muscles in tone. Women with trained pubococcygeus muscles experience orgasm more often than others and give vivid sensations to their partner during sexual intercourse.
Muscle functions in men
A healthy and trained intimate muscle is the key to a man’s sexual health. The health of the prostate gland depends on how much it can contract during sexual intercourse. Its training improves blood supply to the male pelvic organs, without which a normal erection is impossible, and enhances the pleasant sensations during orgasm. The male body produces a sufficient amount of androgens, which contributes to strong potency.
Read more about the functions of the pubococcygeus muscle in men here.
How to do the exercises correctly
The exercises will be most effective if you follow the technique of performing them. Do not over-exert your pelvic floor muscles. If pain occurs, you should stop training.
It is also recommended to focus on the following principles:
- The muscles are out of sight from prying eyes. Therefore, some workouts can be performed while doing your usual activities.
- You should not quit training when the first difficulties appear. As your muscles strengthen, exercises will become easier.
- In parallel with muscle training, it is recommended to practice breathing exercises.
- To achieve the desired result, regular exercise is important. You should not quit training when the first results appear. The optimal duration is 1-2 months. The frequency of training is every day.
- It is recommended to combine more complex exercises with simple ones. This will keep your muscles toned and increase the effectiveness of your workouts.
Guys strive to pump up their womb in order to provide the greatest pleasure to their partner . In men, it takes 2-3 months to pump up the PC muscle. To maintain muscle condition at the proper level, it is advisable to move on to more complex exercises.
The main condition for a successful result is self-discipline. Retention of urination will help check the effectiveness of training. If a man is able to easily stop it for a long time, then the training is not in vain.
Breathing should be smooth and not knocked down, inhalation and exhalation alternate smoothly and are consistent with tension and relaxation.
A sedentary lifestyle and excess weight have a negative impact on the condition of the PC muscle. Moderate physical activity helps strengthen it. Main types of exercises
The training begins with simple exercises. Then more complex ones are practiced. Initially, the muscle should be located. The muscles of the abdominal thighs should be relaxed at this moment. It is necessary to periodically contract and relax the PC muscle, focusing on it.
Preparation for training
After the preparatory activities, it is recommended to perform the following exercises:
- You should tense and relax the muscle 20 times in a row, after which it is fixed in a compressed position for several seconds. Then you need to relax the muscle and take a break for 2-3 minutes. After this, the exercise is repeated. The number of approaches increases over time. It is enough to do this exercise 3 times a week.
- The pubic-coccygeal area slowly relaxes and contracts, each time being fixed in a compressed state for 5 seconds. The number of repetitions is at least 10 times.
- It is required to make the fastest possible movements of the muscle, relaxing and contracting it. These movements are compared to the effect of vibration. A break is taken when a feeling of heat or pain occurs. After 30 seconds you need to do the next approach.
- It is necessary to make massaging movements until the penis is brought into an erection position. Immediately before ejaculation approaches, muscle tension should be exercised, thereby delaying orgasm. After the erection decreases, you should return to massaging. Further actions are carried out according to the described scheme.
- Stepwise contraction of the pubococcygeus muscle is not easy for beginners. The tension occurs gradually, with intermittent movements. When you can no longer strain, you need to fix yourself in this position, and then gradually relax your muscles.
Certain types of exercises are performed during sexual intercourse by both partners. After inserting the erect penis into the vagina, contraction movements with the muscles should be performed without making forward movements.
How to train the pubococcygeus muscle
Kegel exercises are one of the most effective methods of strengthening intimate muscles. They prevent prostatitis in men and uterine prolapse in women. Such gymnastics improves blood supply to the pelvic organs and improves the quality of sensations during intimacy.
These exercises are especially useful for women who have given birth, who often face the problem of urinary incontinence, weakening of the vaginal muscles, and prolapse of the uterus. To correctly perform the gymnastics presented below, you need to feel the location of the muscle. To do this, hold the stream of urine while visiting the toilet. The muscles that tense when performing such an action need to be trained.
Doing exercises
- Lie on your back. Squeeze and release your pubococcygeus muscle 15 times. Every day, increase the number of contractions, bringing their number to 50 in one approach.
- Make the exercise more difficult. Tighten the muscle, hold this position for three seconds, then relax.
- Imagine as if you are pushing something out of your perineum. Try to maintain muscle tension for as long as possible, but do not push too hard.
The exercises presented above should be done once or twice a day. The effect will be noticeable within a month after their regular implementation.
Exercises for the tailbone will also be useful.
Recommendations
This article incorporates public domain text from page 422 of the 20th edition
Gray's Anatomy
(1918)
- Basic clinical anatomy. K.L. Moore and A. Agur. Lippincott, 2nd ed. 2002. p. 217
- Wallner, S., Maas, K., Dabhoiwala, N., Lamers, W., & Deruiter, M. (2006). "Evidence for innervation of the puborectalis muscle by the levator ani nerve." Neurogastroenterol Motil
.
18
(12): 1121–1122. Doi:10.1111/j.1365-2982.2006.00846.x. PMID 17109696. - Drake, Richard; Fogle, A. Wayne; Mitchell, Adam (2015). Gray's Anatomy for Students
(Third ed.). Elsevier. - Christopher R. Chapple (2006). Multidisciplinary treatment of pelvic floor diseases in women
. Churchill Livingston. P. 4–. ISBN 978-0-443-07272-7. - ^ a b c
Grigorescu B.A., Lazaru G., Olson T.R.
et al. (2008). "Innervation of the levator ani muscles: description of the nerve branches to the pubococcygeus, iliococcygeus and puborectalis muscles." Int Urogynecol J Pelvic floor dysfunction
.
19
(1): 107–116. Doi:10.1007/s00192-007-0395-8. PMID 17565421. - Marieb, Elaine (2013). Anatomy and Physiology: Elective Books
. Benjamin-Cummings. item 895. ISBN 9780321887603. - “Core Stabilization, Core Coordination, Article by Aline Newton, MS, Advanced Rolfer Certified, Biomechanics of Core Stabilization, with the Core as the Center of Movement rather than the Center of Containment.” Alinenewton.com. Retrieved 2012-02-20.
- Kegel Exercises Gannet Health Services. Cornwall University website
- How to Do Kegel Exercises (for Men) Silverberg, Corey. About.com
- Dumoulin, Chantal; Hay-Smith, E. Jean C.; Mac Habe-Séguin, Gabriel (14 May 2014). "Pelvic floor muscle training versus no treatment or inactive control for urinary incontinence in women." Cochrane Database of Systematic Reviews
(5): CD005654. Doi:10.1002/14651858.CD005654.pub3. ISSN 1469-493X. PMID 24823491. - Anderson, Coral A.; Omar, Muhammad Imran; Campbell, Susan E.; Hunter, Kathleen F.; Cody, June D.; Glaser, Catherine M.A. (January 20, 2015). "Conservative treatment of urinary incontinence after prostatectomy." Cochrane Database of Systematic Reviews
.
1
: CD001843. Doi:10.1002/14651858.CD001843.pub5. HDL:2164/6141. ISSN 1469-493X. PMID 25602133. - Wallner, S., Maas, K., Dabhoiwala, N., Lamers, W., & Deruiter, M. (2006). "Evidence for innervation of the puborectalis muscle by the levator ani nerve." Neurogastroenterol Motil
.
18
(12): 1121–2. doi:10.1111/j.1365-2982.2006.00846.x. PMID 17109696. - Modi, Rohan M.; Hinton, Alice; Pinchas, Daniel; Groce, Royce; Meyer, Marty M.; Balasubramanian, Gokulakrishnan; Levin, Edward; Stanic, Petr P. (March 2019). "Introduction of a device for modifying defecation posture." Journal of Clinical Gastroenterology
.
53
(3):216–219. doi:10.1097/MCG.0000000000001143. ISSN 0192-0790. PMC 6382038. PMID 30346317. - Sloan, Ethel (2001, p. 53). Biology of Women
, Wisconsin: CENGAGE Delmar Learning. ISBN 0-7668-1142-5 (excerpt available here Archived 2006-05-21 on the Wayback Machine) - Levator Syndrome, Parswa Ansari, MD, 7/2014, Merck Manuals
- Giulio Agnello Santoro; Andrzej Paweł Wieczorek; Clive I. Bartram (27 October 2010). Pelvic floor disorders: imaging and a multidisciplinary approach to treatment
. Springer. item 601. ISBN 978-88-470-1542-5. - Bharucha AE, Trabuco E (September 2008). "Functional and chronic anorectal and pelvic pain." Gastroenterology Clinics of North America
.
37
(3): 685–96, ix. doi:10.1016/j.gtc.2008.06.002. PMC 2676775. PMID 18794003.
Main symptoms of damage
In the absence of regular exercise and prolonged sitting, the pubococcygeus muscle can weaken. The clinical picture indicating damage to the pelvic floor muscles can combine a variety of symptoms. Some doctors combine them into a complex of syndromes that are identical in content, but have different names: coccydynia, levator anus syndrome, coccygeal spasm.
The main symptoms that indicate damage to m. pubococcygeus are:
- urinary incontinence;
- pain when urinating, defecating;
- pain radiating to the coccyx and sacrum;
- feeling of fullness in the rectum;
- decreased libido in women;
- decreased potency, premature ejaculation in men;
- pain in the perineum and vagina in women and in the scrotum in men.
Puborectalis
| Puborectal muscle | |
| The back of the rectum is exposed by removing the lower portion of the sacrum and coccyx. (Puborectalis is not labeled, but the levator ani is labeled bottom right and the external anal sphincter is labeled bottom center.) | |
| Details | |
| Source | lower part of the pubic symphysis, upper fascia of the genitourinary diaphragm |
| Nerve | S3, S4. levator anus[12] |
| Actions | suppress defecation |
| Identifiers | |
| Latin | muscle puborectalis |
| TA98 | A04.5.04.002 |
| TA2 | 2403 |
| F.M.A. | 19087 |
| Anatomical conditions of the muscle [edit in Wikidata] | |
The fibers that form the sling for the rectum are called puborectalis
. They arise from the lower part of the pubic symphysis, and from the upper fascia of the urogenital diaphragm. The puborectalis fibers originate on the posterior surface of the pubis while they are inserted along the midline of the ligation posterior to the rectum. The muscular ligament is innervated by the perineal branches of the S3 and S4 nerve roots.
They meet the corresponding fibers of the opposite side around the lower part of the rectum and form a strong bandage for it. Relaxation increases the angle between the rectum and anus, allowing defecation combined with relaxation of the internal and external anal sphincters. Relaxation of the levator ani and emptying of the rectum are facilitated by anorectal extension during squatting.[13]
Domestic
This group of formations is located in the pelvic cavity. The pelvic muscles include these types of skeletal muscles.
Greater lumbar. This anatomical formation originates on the lateral surfaces of the 1st–4th lumbar vertebrae and the 12th thoracic vertebrae. Its function is external rotation and flexion of the thigh at the hip joint. When fixing the femoral region, this muscle tilts the torso forward, and when raising one leg, it rotates the pelvis around a vertical axis.
Iliopsoas. The psoas major and iliacus muscle bundles take part in the formation of this anatomical formation. The exit point for muscle fibers is a lacuna located in the pelvic region. This anatomical formation forms the lumbar lordosis and the posterior abdominal wall.
Small lumbar. The location of its initial bundles is the lateral surface of the bodies of the 12th thoracic and 1st lumbar vertebrae. The place of its attachment is the crest of the pubic bone. Under the action of the fibers of the psoas minor muscle, tension is exerted on the fascia iliaca.
Pear-shaped. This anatomical structure has a triangular shape and originates on the anterior surface of the sacral joint. This structure is responsible for hip abduction as well as supination.
Obturator (internal). The muscle fibers start from the inner surface of the pelvic bone and extend into the gluteal region. When its fibers contract, the hip abducts. When raising one leg, this muscle prevents the pelvic region from tilting in the opposite direction.